CHAPTER 6 Hallux Varus
DECISION MAKING FOR CORRECTION
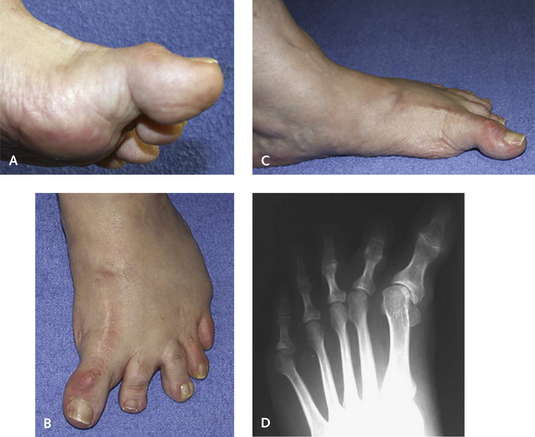
The type of treatment for correction of hallux varus is determined by the flexibility of the metatarsophalangeal (MP) and interphalangeal (IP) joints. Imbalance is always present between the flexor hallucis brevis (FHB) and the extensor hallucis brevis (EHB) muscles and between the abductor hallucis and adductor hallucis muscles. As with any muscle imbalance, the deformity will generally gradually increase, causing a spectrum of fixed and flexible deformities of the MP and IP joints, with or without arthritis of either joint. Fortunately, the IP joint remains flexible in most hallux varus deformities. Over time, however, with increasing imbalance of the FHB and EHB muscles, a contracture of the IP joint develops. If this contracture is rigid or if arthritis of the IP joint is present, an arthrodesis of this joint is usually necessary (Figure 6-1). If an IP contracture is present but the joint is fairly flexible, then I try to manipulate the joint and determine if a tendon transfer without arthrodesis is possible. Release of this contracture generally is not successful because of the contracture of the FHL in addition to tightness of the plantar capsule. Once an arthrodesis of the IP joint is performed, the MP joint deformity must be corrected either dynamically with a tendon transfer or statically through restoration of ligament stability with a tenodesis.
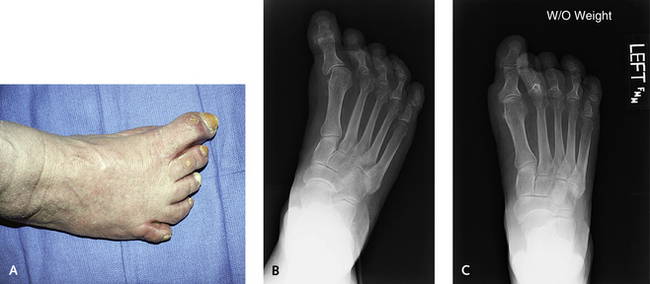
Maintaining MP joint mobility is ideal but not always possible because of arthritis or rigid contracture. Obviously, for a tendon transfer or tenodesis to obtain balance, the joint must be mobile and reducible. At times, however, the flexibility of the MP joint is not clear, and passive correction with manipulation does not clarify the situation. An example is seen in Figure 6-2; in the case depicted, hallux varus is present, and strapping of the hallux into valgus confirmed the flexibility of the joint. This joint reduction must be confirmed radiographically as well as clinically. It is not sufficient to push the hallux into neutral position or even valgus while the patient is seated—the same maneuver should be performed with the patient standing. This assessment will give a far better idea of the dynamic extent of the contracture, when weight-bearing forces are brought to bear on the hallux.
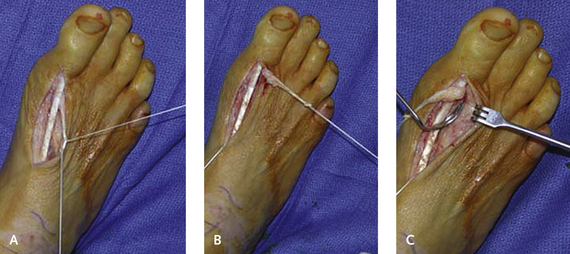
Accordingly, whenever possible, tendon transfer should be used to correct the deformity. However, tendon transfer is contraindicated if either arthritis or rigidity of the MP joint is present. In certain clinical situations, despite apparent flexibility of the MP joint, correction of deformity by restoring soft tissue balance seems implausible. In the case illustrated in Figure 6-3, the patient had a very long first metatarsal with imbalance of the abductor and adductor hallucis muscles. Although an arthrodesis or a resection arthroplasty of the joint can be considered in such instances, my preference would be to shorten the first metatarsal with an osteotomy (a scarf osteotomy is useful here), thereby relaxing the intrinsic contractures, and obtaining further soft tissue balance with a tendon transfer if necessary.
TENDON TRANSFER AND TENODESIS
Tendon Transfers
Various tendon transfers are available for correction of dynamic deformity. The use of the entire extensor hallucis longus (EHL) tendon in conjunction with arthrodesis of the IP joint has been described in the literature, but this is not my preferred procedure. Even if rigid deformity of the IP joint is present and an IP arthrodesis is necessary, I prefer to use half of the EHL for the transfer, maintaining the remaining half as a dorsiflexor of the hallux. If the IP joint is flexible, fusing the joint is unnecessary, and transfer of either a portion of the EHL tendon (a split transfer of the EHL tendon) or the entire EHB tendon is performed (Figures 6-4 and 6-5). Distinguishing a tendon transfer, which has the potential for dynamic correction of deformity, from a tenodesis, in which the tendon is used statically, is relevant here (see Figure 6-5). Both procedures apply to the EHL and EHB tendon transfer, because both may function as either a tenodesis or a dynamic transfer.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree