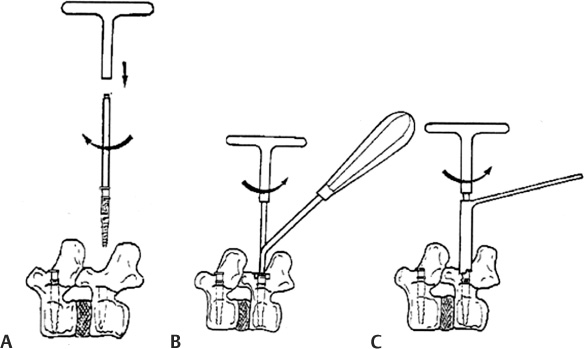
39 Indications for Graf Ligamentoplasty Contraindications for Graf Ligamentoplasty Present: Graf Ligamentoplasty with Anterior Column Support Future: Combination of Rigid and Soft Stabilization Degenerative involution of the spine causes destruction of the spinal stabilizer, which consists of bone, ligament, joint capsule, and disk, which substantially leads to hypermobility and instability of the spine.1,2 As the degenerative changes in the lumbar spine progress, the spinal canal is also compressed by a protruded disk, hypertrophied facet, and ligaments.3,4 In the surgical treatment of such patients, decompression of the spinal canal is mandatory. But the structures, which are removed during decompressive laminectomy, are elements of a stable spine, and postlaminectomy iatrogenic spinal instability may become complicated.5 In patients with preexisting instability or a high risk of postlaminectomy iatrogenic spinal instability, surgical insertion of an internal fixation device as well as spinal arthrodesis were the usual solutions.6–9 The recent development of internal fixation devices such as the pedicle screw fixation system and interbody fusion cages has allowed rigid spinal stability and outstanding surgical outcomes.6,9 However, acquiring stiffness and spinal stability has required the sacrifice of the unique physiological function (i.e., motion) of the spinal segment, which is, without doubt, a disadvantage. Generally, the rigid fixation system has been used to treat lumbar instability. However, it can result in complications such as nonunion, screw loosening, screw fracture, and flat back syndrome.10,11 Rigid fixation also increases the biomechanical stresses on the adjacent segments to the fusion level.12,13 Clinically, the results of several long-term follow-up studies have suggested that spinal fusion might cause deterioration of the adjacent segment.14–16 The complications of rigid fixation have led to the invention of a nonfusion technology that is more physiological than any other fixation devices.17–19 The concept of “dynamic stabilization” is to restrict the hypermobility of an unstable spinal segment rather than eliminating it. Among the types of soft stabilization systems, the Graf soft stabilization system (Sem Co., Montrouge France) was one of the first relatively widely practiced methods.19 The Graf soft stabilization system was invented by Henri Graf.19 It consists of the surgical implantation of a titanium pedicle screw linked with polyester threaded bands as a ligament to connect the pedicle screws across the unstable segment (Fig. 39–1). He believed that instability was related to the development of an abnormal rotatory movement. This abnormal rotatory movement and distraction at the facet joints might be a cause of low back pain. The basic concept is to dynamically stabilize abnormal rotatory movements in physiological lordosis using the Graf band, which results in the alteration of annular and end plate load bearing. This posterior immobilization in lordosis closes degenerative annular tears and degenerative gaps in the facet joint, allowing the healing of damaged tissues.19,20 Figure 39–1 Graf pedicle screws and polyester bands. The Graf soft stabilization system consists of the surgical implantation of titanium pedicle screws linked with polyester threaded bands as a ligament to connect the pedicle screws across the unstable segment. (With permission from Sem Co., Montrouge, France.) Some biomechanical studies using cadavers show that Graf ligamentoplasty reduces the range of motion and provides flexibility under some loading conditions.21–23 Strauss et al21 found that Graf ligamentoplasty significantly reduced range of motion for flexion-extension but had little effect on the translation motion. This finding suggests that Graf ligamentoplasty had the potential to treat “flexion instability.” The advantages of Graf ligamentoplasty are as follows: (1) less invasive, (2) more physiological, (3) reduced biomechanical stress on adjacent segments, (4) no risk of pseudarthrosis, and (5) no donor-site pain.24 The authors think the Graf soft stabilization system gave birth to the concept of dynamic stabilization, making surgeons realize the significance of the ideal stiffness. Undoubtedly, this progress is considered a big leap in the field of degenerative lumbar spine surgery. Our surgical indication for Graf ligamentoplasty is chronic degenerative lumbar disk disorders with or without segmental instability. Each patient has complained about chronic low back pain that has been resistant to conservative treatment over a 6-month or longer period. Initially, degenerative black disk and facet syndrome were included after a specific diagnostic protocol such as diskography and face-togram. However, the clinical outcomes in those entities were not as good. After gaining a certain amount of experience in Graf ligamentoplasty, degenerative black disk and facet syndrome, which Graf initially listed as indications, have been excluded from the indications. In chronic degenerative disk disorder with canal stenosis, Graf ligamentoplasty can be used after decompressive laminectomy or diskectomy, which can prevent postoperative iatrogenic instability, and this turns out to be our major indication. Grade I spondylolisthesis and degenerative slipping (<25%) of the vertebral body might be indications, too. However, we have to be aware that Graf ligamentoplasty is not a procedure that can completely replace spinal fusion and arthrodesis. 1. Chronic degenerative disk disease with or without canal stenosis. 2. Multiple spondylotic lumbar spinal stenosis 3. Lumbar instability syndrome 4. Stabilization of the adjacent segment above or below the main pathology. 5. Degenerative spondylolisthesis (25%) of the vertebral body. 6. Interbody fusion should be added in the following conditions: 1. Isthmic spondylolisthesis 2. Retrolisthesis 3. Degenerative spondylolisthesis greater than grade I 4. Tumors, infection, or trauma 5. Scoliosis deformity 6. Rigid kyphotic deformity The patient operative position is derived from one described by McNab. However, the trunk is placed in a horizontal position with pressure on the upper limbs to obtain an “on-all-fours” position. The cushion is mounted to the table to provide mild support of the rib cage so that it allows the abdomen to be dependent. In this position, the lumbar spine is left in a mean supple lordosis. Care is taken to avoid undue pressure on bony prominences, genitalia, and neurovascular structures. A radiological control allows detection of the involved vertebrae corresponding with the cutaneous guide. A midline linear incision and exposure are made above the involved segments. The surgical approach is made in an assymetrical manner: fixed retractors are replaced by blunt retractors, held by an assistant. After having uncovered the articular area without opening the capsule, the transverse process is exposed. This allows the surgeon to identify the entry for implant insertion. Figure 39–2 Implant placement. (A)
Graf Soft Stabilization: Graf
Ligamentoplasty
 Indications and Contraindications
Indications and Contraindications
Concept and Rationale
Indications and Contraindications
Indications for Graf Ligamentoplasty
 When postoperative iatrogenic instability is anticipated, Graf ligamentoplasty may be indicated.
When postoperative iatrogenic instability is anticipated, Graf ligamentoplasty may be indicated.
 After wide decompressive laminectomy, Graf ligamentoplasty may prevent postoperative iatrogenic instability.
After wide decompressive laminectomy, Graf ligamentoplasty may prevent postoperative iatrogenic instability.
 Especially flexion instability is a good indication.
Especially flexion instability is a good indication.
 Graf ligamentoplasty may reduce the mechanical stress imposed on the adjacent segment.
Graf ligamentoplasty may reduce the mechanical stress imposed on the adjacent segment.
 After diskectomy
After diskectomy
 Modic degeneration
Modic degeneration
 Translational instability
Translational instability
 Narrowed disk height or neural foramen
Narrowed disk height or neural foramen
 When anterior column support is indicated
When anterior column support is indicated
Contraindications for Graf Ligamentoplasty
Operative Techniques
Patient Operative Position
Surgical Approach
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 Concept and Rationale
Concept and Rationale Operative Techniques
Operative Techniques Past, Present, and Future
Past, Present, and Future