and Veronica Tomasello2
(1)
Department of Plastic Surgery and Burns, University Hospital Vall d’Hebron, Barcelona, Spain
(2)
Cannizzaro Hospital, Catania, Italy
Abstract
The bases of vascularised composite tissue allotransplantation rely on general principles of plastic and reconstructive surgery and on modern reconstructive microsurgery. In traditional autotransplantation, soft tissues in the form of flaps or vascularised anatomical parts are autotransplanted to another part of the same patient in order to reconstruct a defect caused by trauma, burns, atrophy or tumour ablation. Nonvascularised grafts survive by diffusion of nutrients until a new capillary network is created. In contrast, flaps do survive by a complete autonomous vascularisation created by microanastomosis between donor and recipient vessels. For years, these types of flaps have been used in reconstructive surgery, especially for head and neck reconstruction, breast reconstruction and lower limb salvage. An important clinical and experimental research has been implemented during the past two decades to provide evidence of the vascularisation of soft tissues and to develop new types of flaps to form and develop modern plastic reconstructive surgery.
Keywords
Face anatomyFacial vesselsFacial nervesClassificationThe bases of vascularised composite tissue allotransplantation rely on general principles of plastic and reconstructive surgery and on modern reconstructive microsurgery. In traditional autotransplantation, soft tissues in the form of flaps or vascularised anatomical parts are autotransplanted to another part of the same patient in order to reconstruct a defect caused by trauma, burns, atrophy or tumour ablation. Nonvascularised grafts survive by diffusion of nutrients until a new capillary network is created. In contrast, flaps do survive by a complete autonomous vascularisation created by microanastomosis between donor and recipient vessels (Fig. 5.1). For years, these types of flaps have been used in reconstructive surgery, especially for head and neck reconstruction, breast reconstruction and lower limb salvage. An important clinical and experimental research has been implemented during the past two decades to provide evidence of the vascularisation of soft tissues (Table 5.1) and to develop new types of flaps (Figs. 5.2 and 5.3) to form and develop modern plastic reconstructive surgery.

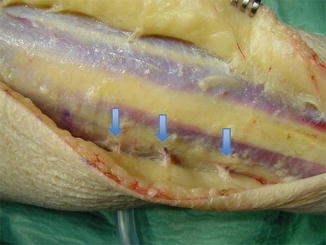
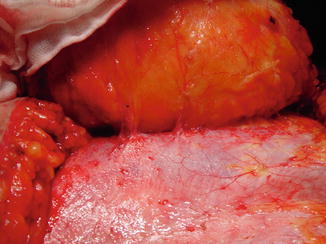

Fig. 5.1
Flaps are the basis of reconstructive microsurgery. Correct anastomosis between flap vessels and recipient’s vessels (either termino-terminal or termino-lateral) is necessary for flap survival
Table 5.1
Common flaps utilised in reconstructive surgery
1. Random local or regional flap (there is not any pedicle identified) |
2. Axial pattern skin flaps (direct arteries to a cutaneous territory; i.e. groin flap) |
3. Fasciocutaneous flaps (fascia, fat and skin, vascularisation through fascial feeders; i.e. radial forearm flap) |
4. Perforator flaps (direct or indirect vessels that pierce fascia/muscle to vascularised soft tissues; i.e. deep inferior epigastric artery perforator [DIEAP] flap) |
5. Muscle flaps (named muscle with its vascular(s) pedicle(s); may include nerve; i.e. latissimus dorsi muscle flap) |
6. Musculocutaneous flaps (Muscle flaps with a skin and fat paddle vascularised through musculocutaneous feeders) |
7. Osteocutaneous flaps (bone and skin ± muscle, through direct vessels and feeders; i.e. fibula flap) |
8. Keystone flaps (locoregional flaps based on fascial/direct perforators/feeders) |
9. Freestyle flaps (free or pedicle perforator flaps based on perforators of any given territory; identified by Doppler and designed ad hoc) |
10. Various: free vascularised nerve flaps, bone flaps, composite flaps, chimera flaps, prefabricated flaps, etc.) |
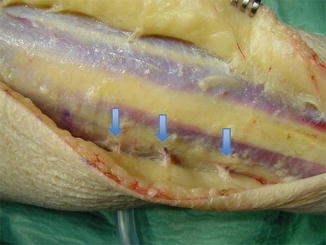
Fig. 5.2
Perforator vessels are the workhorse for new techniques (i.e. keystone flaps, freestyle flaps) and new reconstructive concepts. Arrows signal direct and musculocutaneous perforators
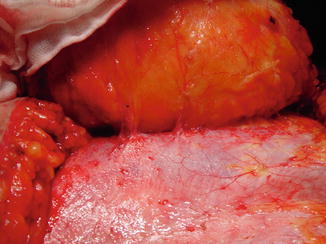
Fig. 5.3
Perforator vessels from the deep epigastric artery and vein form the vascular network for DIEAP flaps, commonly utilised in breast reconstruction
Survival of microvascular flaps depends on an adequate inflow and outflow of vascularisation. It is not only a question of a correct and efficient microvascular anastomosis and good recreation of an anatomical vascular network, but also of a sufficient and balanced blood flow through the entire transplanted tissues. Similarly, functional and sensory recovery relies on neurotisation of muscle units and excellency on neurorrhaphies between donor and recipient nerves that allow scarless neural union that promotes ingrown of axons into the transplanted nerves (Fig. 5.4). The same general principles do apply to face allografts, which depend on a correct vascularisation and functional recovery from different vascular and neural anastomosis between the graft vessels and nerves and recipient vessels and nerves in the cervical and face areas of the recipient. The basis for a robust flap and efficient surgical technique resides on proficiency in reconstructive surgery and anatomic knowledge, often gained in the anatomy room and experimental microvascular lab.


Fig. 5.4
Excellency in microsurgical technique is necessary to obtain good outcomes. Function depends on correct nerve coaptation, similarly to that obtained in face reanimation. Cross-face nerve grafts from sural nerves are anastomosed to face branches on the healthy hemiface and transposed to the contralateral side
5.1 Relevant Anatomy in Face Transplantation
Complete knowledge of anatomy of blood vessels and nerves and other anatomical units in the face and neck region is fundamental for the success of face transplantation. It is very important to understand the microvascular and macrovascular anatomy in order to include the specific vascularisation of any type of face VCA graft in the surgical approach.
5.1.1 Arterial Anatomy
The carotid artery axis is the main arterial network that forms the anatomical basis for face transplantation. Dissection of the common carotid artery is necessary for vascular cannulation in face transplants that receive the preservation fluid infusion in the absence of an intrathoracic approach. Face transplants that require a longer vascular axis for revascularisation require common carotid artery dissection in order to provide an extra length. The internal carotid artery and the vertebral artery do not play any role in face transplantation. They must be preserved, though, to avoid any cerebrovascular risk in the recipient. They do have rich collateral anastomosis, especially the supraorbital artery, supratrochlear and the dorsal nasal artery. The external carotid artery and its terminal branches (in particular face, lingual and superficial temporal arteries) are the main branches for revascularisation and constitute the workhorses for face transplantation (Fig. 5.5).










