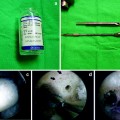
Intrafix
DePuy Mitek, Inc.
Raynham, MA

Image courtesy of DePuy Mitek, Inc.
Bone Mulch Screw
Biomet/Arthrotek
Warsaw, IN

Image courtesy of Biomet Orthopedics, Inc.
WasherLoc
BioMet/Arthrotek
Warsaw, IN

Image courtesy of Biomet Orthopedics, Inc.
Endobutton
Smith & Nephew
Andover, MA

Images courtesy of Smith & Nephew, Inc.
RCI Screw
Smith & Nephew
Andover, MA

Image courtesy of Smith & Nephew, Inc.
SoftSilk
Smith & Nephew
Andover, MA

Image courtesy of Smith & Nephew, Inc.
BioScrew
ConMed Linvatec
Largo, FL

Image courtesy of ConMed Linvatec.
EndoPearl
ConMed Linvatec
Largo, FL

Image courtesy of ConMed Linvatec.
Bio TransFix
Arthrex
Naples, FL

Image courtesy of Arthrex
Metallic TransFix
Arthrex
Naples, FL

Image courtesy of Arthrex
Table 11.2
Available biomechanical data for femoral and tibial fixation devices
Fixation options | Ultimate strength (N) | Stiffness (N/mm) |
|---|---|---|
416–640 | ||
Knotted loop of Mersilene tape [18] | 493 | |
Knotted loop of No. 5 Ethibond [18] | 302 | |
Hamstring graft: femoral fixation | ||
Single: 864–1,086 | 106 | |
Double: 1,324 | ||
1,002–1,235 | 181 | |
746–1,392 | 176 | |
1,112–1,126 | 115–225 | |
DePuy/Mitek metallic cross-pin | 35 mm pin: 1,003 | |
70 mm pin: 1,604 | ||
638–868 | 77–226 | |
352–703 | 8–98 | |
327–539 | ||
310–589 | 26–66 | |
Linvatec Bioscrew with EndoPearl [29] | 659 | 42 |
6 mm soft tissue washers ×2 [30] | 821 | 29 |
Sutures tied over 6.5 mm screw post [30] | 573 | 18 |
20 mm spiked washer with 6.5 mm screw [31] | 248 | |
Hamstring graft: tibial fixation | ||
Mitek Bio-IntraFix [32] | 1,275 | |
796–1,332 | 49–223 | |
903–975 | 87–273 | |
Tandem AO washers/screws [34] | 1,159 | 259 |
Evolgate Device [35] | 1,237 | 168 |
AO washer/screw and sutures around screw post [34] | 768 | 181 |
Tandem bicortical screws with spiked washers [22] | 769 | 69 |
Arthrex 35 mm bioabsorbable screw [33] | 647 | 64.5 |
374–442 | 24–60 | |
Double soft tissue staple [34] | 785 | 118 |
20 mm spiked washer/screw [34] | 724 | 126 |
Linvatec SmartScrew ACL [31] | 665 | 115 |
Linvatec BioScrew [31] | 612 | 91 |
Smith and Nephew SoftSilk [31] | 471 | 61 |
Soft Tissue Graft Fixation
Femoral Fixation
Soft tissue fixation techniques can be divided into two categories: suspensory or compression. Suspensory devices utilize the cortical surface, cancellous surface, or both. A 2006 study of these different types of devices found that cortical-cancellous suspensory fixation had the best biomechanical properties, followed by cortical suspensory fixation and compression devices, which had similar properties, and finally cancellous suspensory fixation with the weakest properties [23] (Table 11.2).
As opposed to suspensory fixation, aperture fixation has theoretical advantages on biologic graft incorporation and can be used in transtibial or anteromedial femoral tunnel preparation. Aperture fixation can be used in the two-incision technique if the outside-in technique is used solely for drilling the tunnel and passing the graft; however, most authors using this technique will fixate the graft on the lateral cortex of the femur. Aperture fixation at the femoral notch side is thought to prevent graft stretching, graft-tunnel motion, and later tunnel widening. Graft-tunnel motion is thought to create a “bungee cord” effect, which may allow an influx of synovial fluid into the tunnel and lead to tunnel widening [37, 38]. In the revision setting, where the tunnel may already be widened, this is of additional concern. Interference screws provide compression of the soft tissue, allowing for direct contact healing with little motion, theoretically improving healing time and preventing a fibrous layer that can be seen with other types of fixation [39]. A recent meta-analysis and systematic review of femoral fixation techniques of soft tissue grafts found a trend toward decreased risk of surgical failure in the interference screw group compared with non-aperture fixation. There was no difference in IKDC values, however [40].
In choosing an interference screw, graft type should be considered. While metal screws allow simple fixation of bone plugs, there is concern that metallic interference screws can lacerate the soft-tissue graft, leading to early failure. A previous study has demonstrated that a metal screw cut or partially cut 9 of 10 grafts with a femoral screw, but 0 of 10 with the tibial screw, indicating there may be some effect of the angle of screw insertion on this finding [41]. The RCI screw was designed to combat this by rounding the threads; however, several studies have found the RCI screw to be biomechanically inferior to bioabsorbable screws in terms of ultimate load, stiffness, and graft slippage [42]. Other studies have found no difference between metallic and bioabsorbable screws in the laboratory setting. Also, a recent meta-analysis of bioabsorbable and metallic screws used in both soft tissue and BTB grafts found no difference in infection, KT-1000/2000, pivot shift, or outcomes scores (IKDC and Lysholm) between screw types. This study comprised 790 knees, and there were no differences other than the bioabsorbable screws creating more joint effusions [43], indicating that if used properly, metal screws may not lacerate the graft [41, 44].
The fixation of soft tissue with an interference screw is dependent on several factors, but tunnel diameter and screw size may be most important. Studies have demonstrated that choosing a screw diameter the same as the tunnel width had improved pull-out strength and minimized graft slippage [45]. Other studies have found that longer screws are better for soft tissue fixation, with 35 mm screws having better biomechanical properties than 28 mm screws [46] and 28 mm screws having better biomechanical properties than 20 mm screws [47]. Decreased soft tissue slippage has been reported when a cortical suspensory device is used in combination with the interference screw. This may be the ideal construct in revision situations in which soft tissue grafts are used as there is increased strength and less slippage with the cortical fixation, yet there is aperture fixation to increase stiffness and eliminate the “bungee effect” that can precipitate further tunnel widening. Also, a larger diameter screw can be used to fill an enlarged tunnel, depending on the technique of femoral drilling. The longest screw length should be selected, although 28 or 35 mm screws may not be possible.
Cross-pin fixation is designed to be used with looped ACL soft tissue grafts, typically hamstring autograft or allograft. This fixation method has not been studied in a revision setting with expanded tunnels; however, cadaver studies with somewhat limited bone quality demonstrated similar fixation strength to bone patellar bone with interference screw fixation [48]. A clinical study comparing a cross-pin device to metal interference screw fixation during primary reconstruction with hamstring tendons found no difference in CA-4000 instrumented laxity measurements or in IKDC, Tegner, and Lysholm outcomes scores. The groups had similar tunnel expansion at 2-year follow-up, which indicates the tunnel expansion may be more related to graft type rather than location of fixation [49]. Another clinical study found no differences in ROM, IKDC, KT-2000, and isokinetic peak muscle torque in four different permutations of Rigidfix (Depuy Mitek, Raynham, MA) femoral fixation, Intrafix (Depuy Mitek, Raynham, MA) tibial fixation, and bioscrew; however, there was significant performance bias as several groups had “back up” fixation with either a button or staple. Another type of cortical-cancellous fixation that has been described, the Ligament Plate (Solco Biomechanical, Seoul, Korea), features cortical screw fixation with a loop that enters the femoral tunnel for graft looping. This device has been found to have similar biomechanical properties of graft fixation as compared to the Endobutton and Transfix (Arthrex, Inc Naples, FL).
Endobutton fixation has long been used for suspensory soft tissue graft fixation, and the newer closed loop version, Endobutton CL (Smith and Nephew, Andover, MA), has been shown to have significantly higher failure load than the original Endobutton, Linx HT hamstring fastener, Bone Mulch screw, Transfix, and bio interference screw [50]. However, the bio interference screw has been shown to have greater stiffness than the Endobutton [51], likely due to its aperture fixation. Comparing cortical suspensory fixation to cortical-cancellous suspensory fixation, a recent biomechanical study found that Endobutton direct (Smith and Nephew, Andover, MA) and femoral Intrafix had similar biomechanical properties to the AXL Cross-pin (Biomet, Warsaw, IN) and Biotransfix II (Arthrex, Naples, FL). In a clinical study with a minimum of 4-year follow-up, 105 patients undergoing primary hamstring autograft ACL reconstruction with Endobutton CL (Smith and Nephew, Andover, MA) fixation, the authors reported no failures related to the femoral fixation and no need for back-up fixation using an interference screw [52].
Another study evaluated the biomechanical performance of several different constructs in terms of maximum failure load, slippage, and stiffness. The constructs tested were Endo Button CL-Bio RCI, Swing Bridge-Evolgate, Rigidfix-Intrafix, Bone Mulch-Washer Lock, Transfix-Retroscrew, Transfix-Deltascrew, and Kryptonite bone cement [53]. The Swing Bridge-Evolgate construct had the highest stiffness and ultimate load to failure, while the Transfix-Deltascrew construct and the Kryptonite bone cement had the lowest ultimate load to failure and were the only two below the 500 N threshold for accelerated rehabilitation. This study had multiple confounding variables despite the authors trying to rectify this by reporting the mode of failure.
Tibial Fixation
Tibial fixation can also be divided into compression fixation and suspensory fixation, which is subdivided into cortical-cancellous fixation and cortical fixation. Compressive fixation via interference screws is also a mainstay for soft tissue graft tibial fixation; however, graft slippage may occur and the interference screw may be more frequently “backed up” when used for tibial fixation of soft tissue grafts. This may be because of the risk of slippage or the ease of visualization of this bone tunnel. Regardless of the reason, this additional fixation increases pull-out strength and decreases graft slippage, and multiple different devices can be used for this back-up fixation. A clinical study in primary ACL reconstructions also noted that hamstring grafts in female patients may have improved Lachman and KT-1000 measurements if reinforced with staples in addition to interference screws [54]. Back-up devices that have been reported include: screw and post, Endobutton, a single staple, dual staples, double spike plate, PLLA ball, biotenodesis screw, cortical disc, cortical screw, and button [24, 55–58]. These back-up devices can each be used as the primary tibial fixation as well.
A second type of compressive device is the Intrafix, which consists of a polyethylene screw and sheath placed within the strands of a soft tissue graft. The screw expands the sheath and wedges the graft against the bone tunnel. Studies again differ in their evaluation of the performance of this device. One study found greater slippage in the Intrafix compared to bioabsorbable screw or a screw and washer type device [59]. However, another study found the Intrafix had higher yield load and stiffness than WasherLoc, tandem spiked washers, Bioscrew, SoftSilk screw, and Smart Screw ACL [60].
Cortical suspensory fixation consists of screw and washer constructs, staples, and the Endobutton. Screw and spiked washer techniques are often used for tibial fixation with soft tissue grafts as they can be used to grasp the graft itself or excess suture from the end of the graft. A tandem washer technique has been described where the sutures are tied in tandem with two washers 15 mm apart; however, various permeations of this technique also include using one of these washers to grasp some of the soft tissue graft. The tandem washer technique and Washer Loc device both achieved ultimate strength well above the minimum 500 N value, but had significantly different values in two different studies [34, 60]. Another screw and washer device, CentraLoc (Arthrotek, Inc Warsaw, IN), has also performed well in biomechanical studies [59].
Cortical-cancellous devices have also been advocated for the tibial graft fixation, including similar cross-pin fixation devices as well as specialized screw and washer devices that penetrate the cortex to fixate the graft to the back wall of the tibial tunnel (WasherLoc). Fixation devices that are placed at the aperture of the tunnel require exacting measurement of graft length to achieve adequate tension which may complicate their use.
Bone Fixation
Femoral Fixation
Interference screws are the mainstay of fixation of a bone plug within a bone tunnel; however, other techniques have been described. Most metal interference screws are now created with titanium due to its relatively inert properties. Bioabsorbable screws initially were created with poly-l-lactide (PLL), which takes years to degrade, if at all. Currently most biodegradable screws are made of some formulation of poly-alpha-hydroxy acids. These biodegradable screws have been cited as having several advantages over metal interference screws, including: less chance of graft laceration [61] if used for soft tissue fixation, no interference with CT or MRI if needed for future meniscal injury or graft failure [62], and the ability to drill through the softer material which negates removal of hardware difficulties in the revision setting [63]. Proponents of metallic screws cite the fact that biodegradable screws are more likely to fracture and have been shown to produce foreign body reactions or persistent sterile effusions within the knee. Recently, biocomposite screws have been introduced. These screws are comprised of varying amounts of tricalcium phosphate and poly-alpha-hydroxy acids, with the claim that there is less soft tissue reaction, faster absorption, and bone ingrowth by 24 months. Another material with increased use is Polyetheretherketone (PEEK), which is thought to be inert and may provide increased strength with similar benefits of being radiolucent and retaining the ability to be drilled [64].
Several studies have found similar results with biointerference screws compared to metal screws [65, 66], with one study finding superior results with metal screws [15




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree