6 Finding the Right Balance: Chemical Peels
Summary
Chemical peels are a mainstay of aesthetic medicine and an increasingly popular cosmetic procedure performed in men. The approach to chemical peels in men includes consideration of intrinsic and extrinsic skin variables that affect various aspects of the peeling process. Owing to the increased sebaceous quality of their skin and thicker dermis, male patients, in general, may require a greater number of treatments, larger volumes of peeling agent, more aggressive degreasing and peel application, and/or higher concentration of peeling agent to achieve optimal results. Patient selection is of utmost importance as poor photoprotective behavior and nonadherence to pre- and postpeel regimens could jeopardize clinical outcomes. The aesthetic clinician with good understanding of men’s cosmetic concerns and a solid foundation on basic and advanced peeling techniques can help the contemporary male patient achieve his desired aesthetics. Chemical peels are safe, cost-effective treatments that provide reliable outcomes and should be an integral part of the aesthetic practitioner’s cosmetic repertoire.
Keywords: chemical peel chemexfoliation chemabrasion male aesthetics trichloroacetic acid phenol-croton oil salicylic acid glycolic acid
6.1 Background
Perhaps the oldest aesthetic procedure performed to date, chemical peeling dates back as early as 1550 BC with the Ancient Egyptians using sour milk, animal oils, salt, and alabaster to aesthetically improve their skin.1,2 In the early 1870s, the first descriptions of chemical peeling in modern medical literature were reported by dermatologists, whose specialty continued to advance the technique throughout the century.2,3
The low-cost and reliable results of chemical peeling have made it a staple procedure in aesthetic medicine. The American Society for Dermatologic Surgery and the American Society for Aesthetic Plastic Surgery reported chemical peels as the fifth most common nonsurgical cosmetic procedure performed in 2017.4,5 An increase of 15.9% compared to the prior year, between 457,409 and 485,371 chemical peel procedures were performed in 2017 totaling $64 million in expenditures.4,5 Men account for only 5.5 and 9.3% of all chemical peel procedures performed in the United States and worldwide, respectively.4,6 Given the growing men’s aesthetic market, chemical peels’ cost-effectiveness in addressing many of men’s top cosmetic concerns make it an essential skill for physicians in aesthetic medicine to develop.7,8,9,10
6.2 Chemical Peels and the Male Skin
6.2.1 Peeling Mechanisms and Classification
Chemical peels induce all three stages of tissue replacement—destruction, elimination, and regeneration—all under controlled inflammation via mechanisms specifically dependent on the peeling agent.11 These peeling mechanisms can be characterized as being primarily caustic, metabolic, or toxic.11 Although a large majority of the medical literature on chemical peeling has regarded acidity as the sole mechanism for peel-induced skin modifications, it is helpful to know that this sole caustic effect only applies to trichloroacetic acid (TCA). As TCA becomes more concentrated, the more acidic it becomes and the deeper it penetrates.11 In addition to dose-dependent cytotoxicity, multiple cellular pathways have been proposed in TCA’s mechanism of action. Platelet-derived growth factor (PDGF) produced by keratinocytes, platelets, and monocytes stimulates wound tissue fibroblast proliferation and integrin expression, which promotes re-epithelialization.12 An inflammatory response involving both proinflammatory cytokine (interleukin-1 [IL-1]) and anti-inflammatory cytokine (IL-10) is also observed. Finally, a local skin equivalent of the hypothalamic–pituitary–adrenal (HPA) axis, known as the skin stress response system (SSRS), has been shown to upregulate pro-opiomelanocortin (POMC) independently of corticotropin-releasing hormone. Apart from melanocyte stimulation, POMC may also be responsible for the controlled inflammation and keratinocyte and fibroblast proliferation after TCA application.13
It has been hypothesized that cellular metabolic effects are partly responsible for the peeling outcomes of alpha hydroxy acids (AHA), such as glycolic and lactic acid, and beta hydroxy acids (BHA), such as salicylic acid (SA). Glycolic acid (GA) at low concentration (< 30%) interferes with sulfotransferases and phosphotransferases on the surface of corneocytes causing corneocyte dyscohesion and subsequent epidermal exfoliation. When used in concentrations such as 30 to 70% free acid in aqueous solution, GA exerts its effect directly based on acidity, detaching cells from each other. Other common peeling substances, such as phenol and resorcinol, work primarily through toxic effects, which cause increased cellular permeability, enzymatic inactivation, and protein denaturation with production of insoluble proteinates. Peeling procedures aim to maintain strict localization of these toxic effects, as other cells distant from where the chemical has been applied can also be affected. Although SA peels work primarily via metabolic mechanisms that cause cells to shed more readily, thereby resulting in keratolysis, it has toxic effects when used in large quantities or large surface areas. Even though they are rarely seen in practice, remembering that SA is made from sodium phenolate, a sodium salt of phenol, may help ensure that the toxic effects of SA are kept in mind and hence potentially avoided.11
Phenol-croton oil’s ability to rejuvenate severely photodamaged skin, surpassing results seen from fully ablative CO2 resurfacing, warrants a brief discussion of its proposed mechanisms. Its active ingredient, croton oil, is derived from Croton tiglium seeds that contain vegetal matrix of 12-myristate-13-acetate and other phorbol esters capable of inducing accelerated deoxyribonucleic acid synthesis and activation of protein kinase C causing extreme inflammatory response.14 Initially thought to be the active ingredient in phenol-croton oil peels, phenol acts a solvent for croton oil allowing penetration of the phorbol esters into dermis where it induces dense dermal neocollagenesis and formation of organized elastic fibers.15,16 These dense neocollagen bands are thicker than those induced by fully ablative CO2 laser and persist decades after the procedure.15,17
Peels that function primarily by metabolic effects generally fall under keratolytics, whereas those that exert their effects via caustic or toxic effects are largely considered protein denaturants.11,18 With these mechanisms in mind, the rationale behind peel combinations and peel selection for specific indications becomes more intuitive. Superficial peels, which are subdivided into very light and light peels, respectively, destroy keratinocytes down to the level of stratum spinosum and stratum basale. Medium peels penetrate into the upper reticular dermis, whereas deep peels wound to the level of the mid-reticular dermis.19 Combining keratolytics with protein denaturants facilitates deeper peel penetration. Classification of common chemical peeling agents and their corresponding depth of penetration is described in Table 6.1.
Table 6.1 Classification of common chemical peel agents and corresponding histologic depth of penetration
Chemical peel classification | Histologic depth of penetration |
Very light superficial •TCA (10–20%) •Glycolic acid (10–50%) •Salicylic acid (20–30%) •Retinoic acid (1–10%) | Stratum spinosum |
Light superficial •TCA (20–30%) •Jessner’s solutiona •Glycolic acid (70%) | Stratum basale |
Medium depth •TCA (35–40%) •Solid CO2–TCA (35%; Brody combination) •Jessner’s solution–TCA (35%; Monheit combination) •Glycolic acid (70%)–TCA (35%; Coleman combination) •Phenol (88%) | Superficial reticular dermis |
Deep •Baker–Gordon phenol-croton oil peelb •Hetter’s phenol-croton oil peel •TCA (> 50%) | Mid-reticular dermis |
Abbreviation: TCA: trichloroacetic acid. aJessner’s solution: 14 g resorcinol, 14 g salicylic acid, 14 g lactic acid (85%), and 100 mL (quantity sufficient to make total) ethanol (95%). bBaker–Gordon phenol-croton oil peel: croton oil, phenol, and hexachlorophene (0.25%). | |
6.2.2 Gender-Linked Skin Differences Relevant to Chemical Peeling
The difference between good and excellent peeling outcomes in men may be attributed in part to a working knowledge of gender-linked differences in skin, as peeling procedures can be very operator dependent and their planning requires careful consideration of multiple factors. The Obagi Skin Classification assesses skin variables such as color, oiliness, thickness, laxity, and fragility to systematically plan pre- and postprocedure skin regimen, select optimal peeling agent, and stratify risks for complication.18 Integrating current research regarding how these variables differ between the sexes may facilitate better peeling outcomes.
Although no gender-linked differences have been reported for melanocyte distribution, intra-ethnic group comparative studies of skin tone show men have darker and less reflective complexions possibly from more vascularized superficial dermis and more melanin.20 Men’s constitutive pigmentation and facultative pigmentation from sun exposure are more robust with longer pigment retention than women.20,21 As will be discussed later, predictable peeling outcomes and common complications from peeling treatment can be anticipated by classifying patients into a genetico-racial skin classification system.22 However, within individual genetico-racial skin groups, men may benefit from longer prepeel skin conditioning and more aggressive photoprotection. Additionally, chromacity studies assessing color differences between erythema and normal skin show higher basal values in men, which may have some implications when evaluating postprocedural erythema.21
Due to androgenic hormone stimulation, it is no surprise that men have higher sebum production that is associated with pore enlargement and predisposition to acne vulgaris.20,21 This propensity for excess sebum production has been associated with impaired stratum corneum barrier function. The increased transepidermal water loss is believed to be related to sebum-induced alterations in intercellular lipid structure and poor corneocyte maturation. Further worsening the barrier function are the behavioral tendencies related to excess sebum in men that result in their avoidance of skin care products due to the perceived fear of exacerbating their already tacky-feeling skin.23 Because of men’s relative oilier skin, a longer or more aggressive prepeel conditioning regimen in the form of stronger topical retinoids and/or more aggressive degreasing may be warranted. Postprocedure acne flares may also be more likely. On the other hand, because men have significantly higher average number of appendageal structures including sebaceous glands, sweat glands, and blood vessels than women, wrinkles may be relatively less prominent in men particularly in the perioral area.24 Because of their higher sebaceous gland density, incorporation of lipophilic peels such as SA and Jessner’s solution (JS) into a male patient’s peel regimen should be given strong consideration if within clinical indication. The higher sebum excretion in men also promotes the growth of Malassezia restricta and M. globosa, which may be indirectly diminished by chemical peeling, thus preventing development or flares of seborrheic dermatitis.25 Facility in performing focal medium to deep peels for sebaceous hyperplasia may also be of value as men may be more likely to seek treatment for this condition.9
Although the extent of differences varies by anatomical region, dermal thickness is greater in men as a result of increased dermal collagen partly from androgen receptor activation.26,27 Differences in study design, measurement tools, sample size, and genetic backgrounds of the subjects may have played a role in some conflicting findings in some studies, but forehead and neck skin are noted to be significantly thicker in men in several studies.21 Similarly, epidermal thickness is greater in the cheeks and back of men. Hence, in order to achieve the intended depth of peel penetration, peeling procedures in men may require higher concentrations and higher volumes of peel solution as well as greater peel application pressure, more peeling sessions, and/or longer prepeel skin conditioning.
Although there are no significant differences in skin elasticity between men and women, lower eyelid sagging is significantly more severe in men starting middle age.28 This finding highlights a potential role for segmental, or targeted, peeling of a specific cosmetic unit, as an early intervention for periorbital rejuvenation in men. Skin microcirculation dysfunction in healthy, middle-aged men in the setting of elevated homocysteine levels may possibly be explained by protective effects of estrogens against homocysteine-induced vascular dysfunction.29 However, in general, higher skin perfusion is observed in men than in women.30,31 The larger number of microvessels in the male face could in theory make men more susceptible to medium- and deep peel–associated persistent erythemas, which result from angiogenic factors stimulating vasodilation. This is a sign of prolonged phase of fibroplasia, which may lead to scarring.32 Although men may be more likely to tolerate pain from chemical resurfacing,33,34 androgen-associated diminished re-epithelialization rates may extend their expected downtime for these procedures.35,36 Furthermore, more robust histamine response is observed in men and older age patients.37 This has clinically significant implications especially in periorbital rejuvenation via medium or deep peeling in men, where significant edema may cause the eyes to swell shut but may be mitigated by aggressive prophylaxis and treatment with antihistamines.38 Table 6.2 summarizes male-specific intrinsic skin variables and relevant peeling considerations.
Table 6.2 Intrinsic skin variables in men and relevant peeling considerations
Gender-specific skin-related variables | Peeling considerations |
Color •Robust facultative pigmentation after sun exposure | •May require longer pretreatment •Higher risk for PIH → need more aggressive photoprotection |
Oiliness •Higher sebum production •Predisposition to acne vulgaris •Avoidance of face products due to fear of worsening tacky skin sensation | •May require longer pretreatment and more potent topical retinoids •Must aggressively degrease (hard “scrub” as opposed to “wipe”) •Better candidates for lipophilic peeling agents (e.g., salicylic acid) •High risk for postpeel acne flare → consider continuing or restarting oral acne meds •Poor skin barrier function → need more counseling on consistent daily skin regimen |
Thickness •Increased dermal collagen in men due to androgen receptor activation •Thicker epidermis | •May require longer pretreatment and more aggressive degreasing •Commonly need higher volumes and higher concentrations of peeling agent •Firmer peel application pressure •More treatment sessions needed |
Elasticity •Lower eyelid sagging presents much earlier | •Discuss the role of segmental peels in periorbital rejuvenation and offer such intervention earlier and in combination with other minimally invasive procedures |
Pain perception •Ablative CO2 laser-evoke potentials are lower in amplitude than females suggesting better pain tolerance | •May require less aggressive pain management (although individual variation likely) |
Re-epithelialization rate •Slower wound healing due to androgens | •Set realistic expectation regarding postprocedural downtime |
Histamine response •More robust response in men and increasing age | •Aggressive antihistamine prophylaxis to mitigate postprocedural edema especially in periorbital rejuvenation with medium or deep peeling agent |
Abbreviations: PCP, primary care provider; PIH, postinflammatory hyperpigmentation. | |
6.2.3 Men and Extrinsic Factors Relevant to Chemical Peeling
Men may be more likely to avoid healthy skin care practices, as previously alluded to when discussing men with higher skin sebum content having poor skin care regimen.23 They may also participate in behaviors that contribute to signs of aging, with smoking and ultraviolet (UV) light exposure being of most significance.39 Because of higher risks for suboptimal peeling outcomes and worse complications, peeling procedures in patients who fail to modify these behaviors should be approached with extreme caution or not be attempted at all.40
The latest age-standardized worldwide prevalence of daily smoking for men is 25% compared to 5% for women.41 In the United States, the most recent prevalence estimates are 21.7% for men versus 18.4% for women.42 Factors such as vasoconstriction, increased oxidative damage, inhibition of fibroblastic activity, and upregulation of matrix metalloproteinases have been proposed as potential mechanisms of how tobacco exposure accelerates skin aging.43 As a well-known risk factor for wrinkle development,44 strong emphasis should be placed on smoking cessation when counseling men prior to any peeling procedure. The potentially increased risks for scarring and poor wound healing associated with tobacco exposure may lead to disastrous peeling outcomes.45
Outdoor occupations are overwhelmingly comprised by men.46 To add to this occupational risk factor for UV radiation skin damage, men, including those already at high risk of skin cancer, are less likely to practice sun protective behaviors despite male skin’s reduced antioxidant capacity and increased tendency for UV-induced immunosuppression.47,48,49,50 Although each patient is unique, in light of these findings, men may be at a higher risk of chemical peel-associated postinflammatory hyperpigmentation (PIH) and may require longer skin prepeel conditioning. Postprocedure skin care regimen, including possible work-related UV exposure restrictions, must be discussed explicitly. Considering chemical peels’ proven benefit in actinic keratosis (AK) reduction and skin cancer prevention,51 careful patient selection is of utmost importance.
Finally, peeling practitioners should be familiar with current research on men’s preferences regarding skin care products.52 In general, gender does not play a significant role in treatment adherence in dermatology except for acne where males have a reportedly lower adherence rates.53 However, knowledge of men’s preferences toward particular skin care products may prove advantageous in increasing likelihood of product utilization. Men tend to be very aggressive when they scrub, a habit that men may regard as a physical cue that the product is working. In the United States, men gravitate toward products that create a perception of “refreshing and reviving tired skin.”52 Cleansers that run thin and are clear blue or green with suspended bubbles are well liked by men. Similarly, men prefer emollients with lighter, airy feel to the skin as opposed to thick, opaque creams.52 Familiarity with new and existing skin care products that fit these general principles may improve peeling outcomes in male patients by having a framework to select effective pre- and postpeel skin care products that men are more likely to use. Table 6.3 summarizes male-specific extrinsic skin variables and relevant peeling considerations.
Table 6.3 Extrinsic skin variables in men and relevant peeling considerations.
Gender-specific skin-related variables | Peeling considerations |
Smoking •More prevalent in men (25%) than in women (5%) | •Discuss resultant accelerated aging, poor wound healing, and increased scarring risks → counsel on smoking cessation •For deep peels, at least 1-y cessation recommended |
Ultraviolet radiation exposure •Higher occupational risks •Inadequate photoprotective behavior •Reduced skin antioxidant capacity | •Increased skin cancer risks → discuss benefits of chemical peeling for actinic keratosis reduction/skin cancer prevention •May need additional counseling on photoprotective behavioral modification |
Facial cleansing habits •Aggressive scrubbing quite common | •Counsel on gentle skin care practices •Emphasize high risks for scarring if aggressive exfoliation is performed postpeel |
Skin care product preferences •Cleansers: thin, clear blue or green with suspended bubbles •Emollients: preference for less occlusive vehicles | •Always consider vehicle preferences when recommending pretreatment or other skin conditioning medication (e.g., adapalene 0.3% gel may be preferred to tretinoin 0.1% cream) •For medium or deep peel postprocedure emollients, explain the barrier function rationale for using occlusive vehicles, which may ensure adherence |
6.2.4 Peel Considerations in Sexual Minority Men
More than 10 million adults in the United States identify as lesbian, gay, bisexual, and transgender (LGBT), with 3.9% of men identifying as belonging to this group.54 Ongoing efforts throughout medicine and within the dermatology specialty have been put forth to bridge the gap in LGBT health.55,56 The literature specifically addressing chemical peel considerations in sexual minority men appears even more scant than their heterosexual or cisgendered counterparts. This subsection aims to synthesize known epidemiological, behavioral, and physiological data pertaining to sexual minority men that are relevant to chemical peeling procedures (Table 6.4).
Table 6.4 Peeling considerations in sexual minority men
Skin-related variables in sexual minority men | Peeling considerations |
Transgender men on cross-hormone testosterone therapy •Acne vulgaris on face and trunk peak after 4–6 mo of therapy | •Consider serial salicylic acid peels as adjunct to standard acne treatment •For body peeling: consider salicylic acid in polyethylene glycol vehicle given lower absorption and decreased risks for salicylism |
Gay and bisexual men Ultraviolet (UV) exposure •Indoor tanning 6 times more prevalent than heterosexual counterpart Anabolic androgenic steroid use •More prevalent among ethnic minority gay and bisexual men and adolescents •Unlikely for many to openly discuss steroid misuse | •Photoprotective behavior counseling should focus on concepts of UV-associated accelerated aging/wrinkle formation •Serial chemical peeling may circumvent need and associated risks from using oral antibiotics to improve acne in patients concomitantly on anabolic steroids |
In comparison to their heterosexual counterparts, homosexual men are more likely to consider noninvasive and invasive cosmetic procedures and, in general, are more open to disclosing their experience with these procedures.57 Indoor tanning is up to six times more common in gay and bisexual men than in heterosexual men.58,59 Those who perceive their skin tone as not matching their darker ideal skin tones were more likely to engage in indoor and outdoor tanning, the highest of which were among light-skinned individuals.60 These findings may make sexual minority men more likely to seek out resurfacing procedures such as chemical peels while being at high risk of behaviors that could negatively impact peeling outcomes or even exclude them from being candidates for chemical peels. Discussion and implementation of UV exposure behavior modification may be more seamless in sexual minority men whose culture may value lighter skin, although future research into this is necessary. Nevertheless, emphasizing wrinkle and skin aging prevention may effectively deter sexual minority men from engaging in UV exposure61 that could jeopardize their candidacy and/or the outcomes of their chemical peeling procedure.
Transgender men undergoing cross-sex hormone treatment with testosterone commonly develop acne vulgaris, with up to 94% of patients developing acne on the face, chest, and back within 4 to 6 months of testosterone initiation.62,63 In most cases, acne decreases in severity a year after testosterone therapy initiation and a majority are responsive to topical retinoids and topical/oral antibiotics.62,64 Face and/or body peeling using serial SA and other peels65 should be considered as they can offer immediate and reliable improvement of comedonal and inflammatory acne.65,66 Severe cases may require treatment with isotretinoin, which involves nuanced comprehension surrounding the need for contraception and pregnancy testing in this population.56,63 Superficial peels such as SA or JS may still be safely performed in patients concomitantly on isotretinoin and may serve as an effective adjunctive treatment.67,68
A higher prevalence of anabolic androgenic steroid (AAS) use is reported among sexual minority men in comparison to their heterosexual counterparts.69,70,71 Moreover, AAS misuse among sexual minority adolescent boys is three to four times higher than in heterosexual boys, especially among Black and Hispanic males.72 Although addressing misuse of AAS in these populations is beyond the scope of this chapter, similar peeling recommendations as discussed in transgendered men apply to this group and may improve self-esteem.73
6.3 Approach
6.3.1 Indications
As with any aesthetic procedure, proper patient selection, preoperative consultation, and procedural planning is tantamount to positive outcomes. Indications for chemical peeling in men (Table 6.5) is very similar to women although some conditions may be more commonly observed in men, such as pseudofolliculitis barbae. It is crucial to understand the histopathologic changes present in the condition to be treated and the depth at which they occur in the skin as peeling agent(s) can be tailored to specifically address these issues. UV light examination can further assist in determination of level of pigment deposition. Moreover, patient photography under this lighting can illustrate the severity of patient’s photodamage and subsequent improvements after treatment.74,75 In general, the more superficial the skin pathology, the more responsive it is to a chemical peel; hence, deep wrinkles, as commonly seen in men, do not respond to peels as adequately and as readily as fine, superficial wrinkles.22
Table 6.5 Summary of chemical peel indications for men and corresponding peel selection
Indication | Example of peel selection | Practical considerations |
Acne vulgaris and scarring Comedonal and mild/moderate inflammatory Truncal acne or skin of color patients Rolling acne scars Ice pick and/or boxcar acne scars | Salicylic acid (20–30%) Glycolic acid (70%) Salicylic acid (30%) in polyethylene glycol Salicylic acid (30%) + TCA (10–20%) Combination medium-depth TCA peels (e.g., Brody combination) CROSS method TCA (50–100%) CROSS method phenol-croton oil (88 and 4%, respectively) | Combine with other modalities: microneedling, PDL, subcision, erbium glass laser Polyethylene glycol vehicle may decrease risk of salicylism and postinflammatory hyperpigmentation (PIH) prone “hot spots” |
Rosacea Erythrosis Papulopustular | Salicylic acid (20%) Salicylic acid (20–30%) | 1 application 2–3 applications |
Keratosis pilaris | Glycolic acid (50–70%) | Daily maintenance therapy with glycolic acid lotion (12–20%) 48-h postpeel |
Melasma, PIH | Salicylic acid (20–30%) ± TCA (10%) Glycolic acid (50–70%) TCA (10–30%) Phenol-croton oil peels (light or very light Hetter’s formulation for resistant cases) | Perform at 2-wk intervals May start at lower glycolic acid concentrations (30%) for PIH |
Actinic keratosis | Salicylic acid (30%) + TCA (10–35%) Jessner’s solution + spot TCA (35%) Glycolic acid (70%) | May pretreat with 5-FU (5%) cream × 1 wk or perform as “pulse peels” |
Dermatoheliosis/periorbital rejuvenation •Mild photoaging •Moderate to severe photoaging | Jessner’s solution Glycolic acid (70%) Salicylic acid (30%) + TCA (10%) Jessner’s-TCA (35%) Solid CO2-TCA (35%) Glycolic acid (70%)-TCA (35%) Hetter’s phenol-croton oil Phenol (88%) in micropunch blepharopeeling | Use in combination with other minimally invasive procedures including neurotoxins, fillers, microneedling, and/or skin-tightening devices Segmental peeling (not full face) recommended when using phenol-croton oil in men due to difficulty camouflaging postprocedural erythema without makeup |
Pseudofolliculitis barbae | Salicylic acid (30%) Glycolic acid (50–70%) Jessner’s solution | Repeat every 2–4 wk as needed |
Abbreviations: 5-FU, 5-fluorouracil; CROSS, chemical reconstruction of skin scars; PDL, pulsed dye laser; TCA, trichloroacetic acid. | ||
6.3.2 Prepeel Consultation
A comprehensive prepeel consultation is crucial to ensure that both the physician and patient have communicated their expectations and risks and benefits are appropriately discussed. A thorough history should be obtained with the aim of identifying factors that can impact wound healing. Any pathologic process or medication that alters the health or density of pilosebaceous units may impair proper skin re-epithelialization. Systemic illness or postoperative status affecting overall nutritional state, such as in the case of postbariatric surgery patients, should be assessed as these may limit proper wound healing. A history of PIH or hypertrophic or keloid scarring should be assessed. Prior history of herpetic infection or recurrent staphylococcal infection facilitates proper planning for prophylactic medications.
Although superficial chemical peels may be safely performed during or within 6 months after isotretinoin therapy, current evidence precludes recommendation on the use of medium or deep chemical peels while on isotretinoin.67,68 The reported and potentials risks of concomitant isotretinoin and medium/deep peels should be discussed thoroughly with the patient. Patients with acne concurrently on oral antibiotics such as doxycycline may continue therapy, although discussion about photosensitivity should be emphasized. Similarly, increased risk of hyperpigmentation should be discussed in patients on minocycline. Concurrent exogenous testosterone use may portend the need for ongoing serial chemical peeling procedures.
Psychiatric disorders such as depression, body dysmorphic disorder, or obsessive compulsive disorders should be screened, as adequate management by mental health specialists is necessary prior to proceeding with a chemical peeling procedure. Even when outcomes are successful objectively, patients undergoing a peel for barely noticeable skin anomalies are likely to be unhappy with postoperative results.18 As extensively discussed in the prior sections, gender-specific extrinsic factors relevant to peeling such as UV radiation (recreational outdoor, occupational, or indoor tanning) exposure should be thoroughly assessed.
General absolute contraindications to chemical peels in men include active infection and allergic contact dermatitis to peel ingredient(s). Relative contraindications include smoking, regular indoor or outdoor tanning, history of PIH, history of poor wound healing, history of high-dose iatrogenic immunosuppression (e.g., for treatment of autoimmune disease or transplant rejection), active inflammatory dermatoses, cardiac, renal, or hepatic disease (for phenol-based peels), and habitual excoriation. Absolute contraindications to phenol-based peels include history of hypertrophic scarring or keloid formation, Fitzpatrick skin type VI, and recent surgical rhytidectomy, as vascular compromise and scar formation can occur when deep peel is applied to recently undermined skin.75 No more than 5% body surface area (BSA) should be treated with phenol in a single session. The recommended single-session phenol peeling maximum total BSA treated is 2% in those with underlying cardiovascular disease.76 Transient rate-corrected QT interval (QTc) prolongation may occur during phenol-croton oil peel; thus, medications known to prolong QTc should be discontinued especially in those undergoing full-face or multiple segmental phenol-croton oil peel.16,77 In addition, some peeling experts recommend smoking cessation for at least 12 months prior to any deep peeling procedure.76 A summary of absolute and relative contraindications to chemical peels in men is listed in Table 6.6.
Table 6.6 ontraindications to chemical peeling in men
Absolute contraindications | Relative Contraindications |
Active infection at the treatment area History of keloid at the treatment area Allergic contact dermatitis to peeling agent to be used Ehlers–Danlos syndrome Habitual excoriation, emotional instability, or mental illness Inability to follow instructions Unrealistic expectations | Active rosacea and other inflammatory dermatoses Vitiligo Nutritional deficiencies (e.g., from bariatric surgery) Diabetes Isotretinoin use within 6–12 moa History of radiation to treatment area Iatrogenic immunosuppression Scleroderma or other collagen vascular disease History of herpetic infections Significant hepatic/renal/cardiac diseasea Recent rhytidectomya Darker skin types (Fitzpatrick skin type VI)a Smoking/vaping/nicotine use Job- or recreation-related anticipation of inadequate photoprotection |
aMore relevant when performing deep peeling. | |
Ideal peel candidates should be both willing and actually adherent to pre- and postpeel care regimen. Poor adherence to prepeel skin conditioning could be a telltale sign of inability to closely follow postoperative instructions. Men who work or regularly exercise outdoors may present a relative contraindication depending on the patient’s ability and/or willingness to avoid sun exposure of the treated area postpeel. Although there are no absolute contraindications for periorbital peeling, unless corrected prior to the chemical peel, preexisting ectropion or moderate to severe lower lid laxity are relative contraindications for lower eyelid peeling.78 If a lag or ectropion is observed after the lower lid is pulled down away from the globe for several seconds (snap back test), deep peeling the lower eyelid with phenol-croton oil can lead to an ectropion.75,76
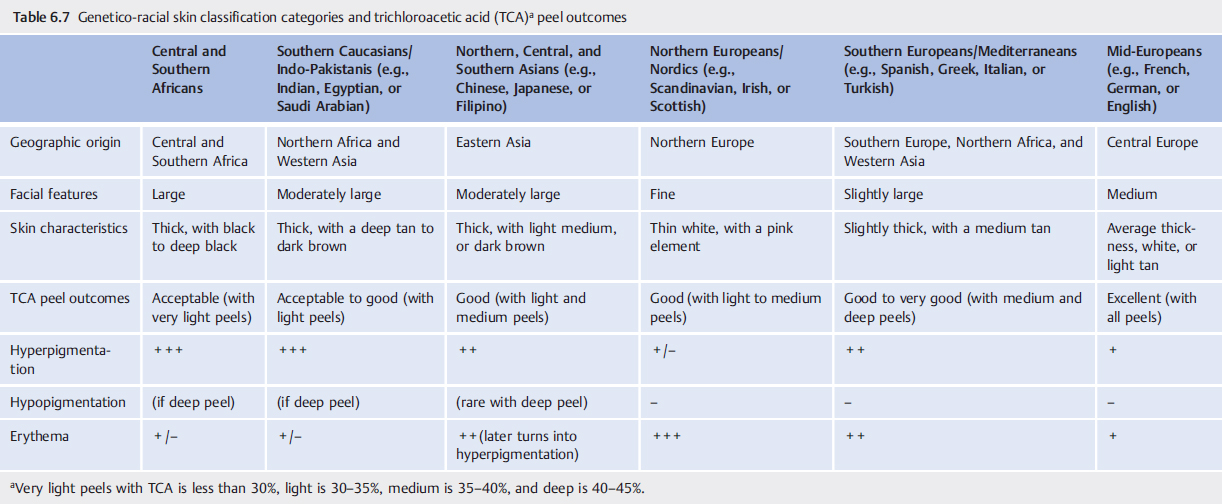
Skin type assessment is an integral part of the prepeel consultation. Common classification has been primarily based on degree of skin pigmentation and tanning/burning susceptibility. However, more reliable skin type classification for chemical peeling has been proposed by Fanous and Zari that utilizes a genetico-racial category (Table 6.7).22 Inhabitants from the three ancient continents—Europe, Africa, and Asia—exhibit predictably lighter, thinner skin and smaller features as one moves north, and gradually display darker, thicker skin with larger features as one moves south. In this classification, Europe and Africa run in a parallel vertical fashion to Asia and is divided into six total categories. By using this genetico-racial classification, peel outcomes can be reliably predicted, and complications are more likely to be prevented. For example, despite their Fitzpatrick phototype, it may not be advisable to proceed with a deep peel in Nordics (e.g., Scandinavian, Irish, or Scottish) as their thin skin may make them prone to scarring. A useful peeling guideline that incorporates this genetico-racial classification is as follows: (1) medium to deep peels for mid-Europeans and southern Europeans (Mediterraneans), (2) medium and light to medium peels for northern Europeans (Nordics) and Asians, (3) light peels for southern Caucasians (Indo-Pakistanis), and (4) very light peels for Africans.
6.3.3 Prepeel Skin Conditioning
Proper skin conditioning prior to a peel, also called skin priming, is essential to a successful chemical peeling outcome. The overall goal of skin priming is restoration of skin back to a normal state prior to wounding it.79 This is achieved by thinning the stratum corneum, melanocyte regulation, and dermal collagen production. These processes facilitate uniform peeling agent penetration, prevention of postinflammatory dyspigmentation, and predictable and more rapid re-epithelialization.
Skin priming may be divided into two phases: pretreatment and preparation.80 Pretreatment includes the days up to months before the peeling procedure. Preparation consists of the steps performed immediately before the peeling procedure, which include degreasing and application of topical anesthesia, as needed. Due to various intrinsic and extrinsic factors previously discussed, men may require longer pretreatment regimen as well as more aggressive skin preparation. Agents used during the pretreatment phase can include topical retinoids (tretinoin, retinaldehyde, adapalene, or tazarotene), keratolytics (lactic acid, SA, kojic acid, or GA), and lightening agents (hydroquinone or azelaic acid; Table 6.8). Because men gravitate toward simple, quick therapeutic strategies, their adherence to regimens that entail multistep daily routines may be dismal.81 Since convenience and simplicity are key for men, agents already commercially available in combination or an individually compounded topical prescription may be more ideal. Typical pretreatment begins 4 to 6 weeks prior to planned chemical peeling; however, skin of color patients may require 8 to 12 weeks.74 A common skin priming regimen involves compounded hydroquinone (8%), tretinoin (0.025%), and hydrocortisone (1%; modified Kligman’s formula) at night for the entire pretreatment period.80 For genetico-racial groups at risk of postpeel hyperpigmentation (Table 6.7), as well as those with history of dyschromia, expert consensus recommends cessation of topical retinoid 1 week prior to chemical peel in order to prevent potential peel overpenetration.82–84 Particularly for GA peeling, there may be value to incorporating a topical cream or lotion containing 8 to 10% GA in the patient’s at home priming regimen, as unusual sensitivity to GA may be unmasked, allowing the peeling practitioner an opportunity to select a more appropriate peeling agent.85 In contrast, there are differing views among peeling experts regarding the importance of pretreatment prior to deep peeling with phenol-croton oil.40
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree