Chapter 1
FACIAL ANATOMY
STRUCTURAL PLANES OF THE FACE
A complete knowledge of the gross anatomy of the face is crucial to choosing, and safely performing, proper invasive surgical procedures. Every technique discussed later in this book is easier to understand and then apply if the underlying anatomical principles are firmly in the reader’s mind. This chapter is a discussion of the anatomy of the head and neck as it applies to oculoplastic aesthetic and reconstructive surgical intervention. A more detailed discussion of the eyelid anatomy is included.
The structural planes of the face will be discussed first and include: (1) the skin; (2) the superficial facial fascia; (3) the mimetic muscles; (4) the deep facial fascia; and (5) the plane containing the facial nerve, parotid duct, and buccal fat pad. The anatomy of the facial ligaments, vessels, lymphatics, and bones as they relate to surgical procedures of the face will also be presented.
The eyelids are of special interest to the oculoplastic surgeon and will be discussed in significant detail in the second section of this chapter.
SKIN
The skin is the largest (though not the heaviest) organ of the body. In addition to providing a barrier to physical injury and infection, the skin also has psychosocial and aesthetic importance. This is especially true in the face. The surgeon who undertakes surgical manipulation of the face should have a clear understanding of the anatomy of the skin and its response to injury (i.e., wound healing).
Basic Anatomy
The skin consists of three layers: epidermis, dermis, and subcutaneous fat (Fig. 1-1).
The epidermis is an integrated epithelial layer of four distinct, contiguous zones (basal, spinous, granular, and cornified layers) that are apparent with light microscopy. It completely replaces itself every 12 to 14 days. The basal layer is the main proliferative compartment of the epidermis. The immediate suprabasal keratinocytes make up the spinous layer, so named because of the “spiny” projections that span their intercellular spaces to adjacent cells. Ultrastructurally these are recognized as desmosomes. The granular layer comprises the two to three cell layers found between the spinous and cornified layers. These cells participate in the cornification process by releasing their lipids into the intracellular spaces. This enhances the skin’s barrier function and aids in intracellular cohesion within the stratum corneum. The cornified layer(stratum corneum) is the most external layer furthest from the dermis. It is thinnest on the eyelids and the genitalia. Desquamation occurs here with loss of desmosomal connections.
Melanin is produced in pigment granules known as melanosomes that are synthesized in melanocytes and passed to the epidermal cells in the deeper layers of the epidermis. An epidermal melanin unit consists of a melanocyte in contact with ~ 36 keratinocytes. There are no significant differences among races in the number or distribution of melanocytes. The skin color is determined by the amount of melanin present in the skin as well as by its distribution. Black skin is darker because of increased production, distribution, and retention of melanin, not a greater number of melanocytes.
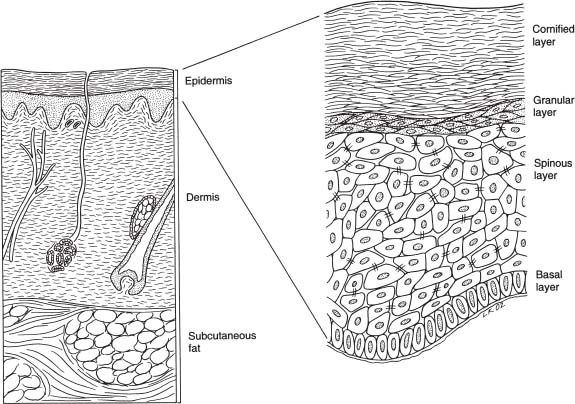
FIGURE 1-1 Skin with three layers: (1) epidermis, (2) dermis, and (3) subcutaneous fat.
The major structural component of the dermis is collagen, of which Type I and Type III are the most predominant. Type I accounts for ~ 80% of the total collagen in human skin. The superficial papillary dermis contains thin, randomly arranged collagen fibers, mainly of Type III. The deeper reticular dermis has coarser collagen bundles that run parallel to the surface of the skin. The dermis also contains blood vessels, lymphatics, nerves, and epithelial adnexa (hair follicles and sebaceous, apocrine, and eccrine glands).
Elastic fibers make up ~ 3% of the dry weight of the dermis. Ground substance is an amorphous material (made up of water, electrolytes, plasma proteins, and mucopolysaccharides) that fills spaces between the cellular and fibrillar components of the dermis.
Subcutaneous fat lies beneath the dermis. The thickness varies from individual to individual and from one area of the face to another. The cheeks, temples, and neck have the thickest subcutaneous fat pad. Connective tissue septa divide the subcutaneous fat into lobules.
A plane of submuscular, nonseptate fat exists. A supraperiosteal submuscular fat pad, the suborbicularis oculi fat (SOOF), is present over the zygoma and maxilla (Fig. 1-2). This is continuous superiorly with the retro-orbicularis fat (ROOF) situated in the eyebrow fat pad described by Lemke and Stasior and extending a variable amount into the upper eyelid.
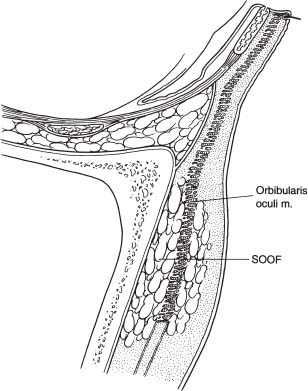
FIGURE 1-2 Suborbicularis oculi fat (SOOF). A supraperiosteal submuscular fat pad.
SUPERFICIAL FACIAL FASCIA
The superficial facial fascia, which is an extension of the superficial cervical fascia in the neck, along with the facial mimetic muscles (platysma, zygomaticus major, zygomaticus minor, and orbicularis oculi) that it invests, makes up the superficial musculoaponeurotic system (SMAS) (Fig. 1-3). The SMAS is relatively thick over the parotid gland, and it thins as it extends medially. In the upper lip, it essentially represents the epimysium of the elevators of the lip. It extends superiorly as the temoral parietal fascia. The only difference in this temporal area is the absence of a mimetic muscle. The SMAS acts as a distributor of facial muscle contractions to the skin. Facial expression results from the contraction of the mimetic muscles. These muscle actions are then transmitted to the skin by ligamentous attachments located between the SMAS and the dermis. These fibrous septa divide the subcutaneous fat into lobules. In general, the facial skin is supported by retaining ligaments that extend from a deep, fixed structure to the overlying skin. These will be discussed later in this chapter. Over time, the effects of gravity and age cause relaxation and laxity of facial soft tissues. Facial surgeons routinely perform a SMAS dissection during facial rejuvenation procedures to correct SMAS ptosis. The SMAS thus has important implications for cosmetic surgery and rhytidectomies.
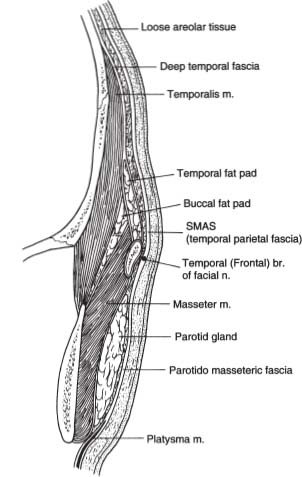
FIGURE 1-3 Superficial musculoaponeurotic system (SMAS). A superficial facial fascia.
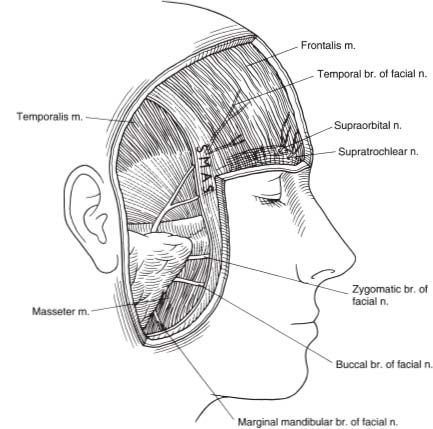
Major vessels and nerves are deep to the SMAS, and their smaller branches perforate it (Fig. 1-4). The subdermal plexus lies superficial to the SMAS. There are important regional variations in the anatomy of the SMAS and associated neurovascular structures.
In the lower face, the facial nerve branches are deep to the SMAS, as are the sensory nerves. The facial muscles receive their innervation on their deep surfaces with the exception of the deeply situated buccinator, levator anguli oris, and mentalis. Dissections superficial to the SMAS protect these structures.
In the temporal area, the temporal branch of the facial nerve crosses the superficial aspect of the zygomatic arch and continues within the temporal parietal fascia (or SMAS of upper face) to its entrance into the frontalis muscle (see Fig. 1-4). The only difference anatomically between the SMAS of the lower face and that in the temporal region is the absence of mimetic muscle in the temporal parietal fascia.
In the upper face, the superficial supraorbital and the supratrochlear neurovascular bundles exit their respective foramina, penetrate the SMAS, and course superiorly beneath the skin’s surface. The deep branch of the supraorbital nerve remains deep to the frontalis muscle in the submuscular fascia. Dissections beneath the temporal parietal fascia (or SMAS of upper face) temporally protect key neurovascular structures.
MIMETIC MUSCLES
The mimetic muscles can be grouped into superficial and deep. Superficial mimetic muscles, which receive their neurovascular supply to their posterior surface, include the orbicularis oculi, platysma, zygomaticus major, zygomaticus minor, and risorius.
Deeply situated mimetic muscles, which receive their neurovascular supply to their anterior surface, include the buccinator, mentalis, and levator anguli oris.
FIGURE 1-4 Nerves that are deep to the superficial musculoaponeurotic system are noted.
Facial musculature can be divided into two other groups: (1) facial expression and (2) mastication.
Facial Expression
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree