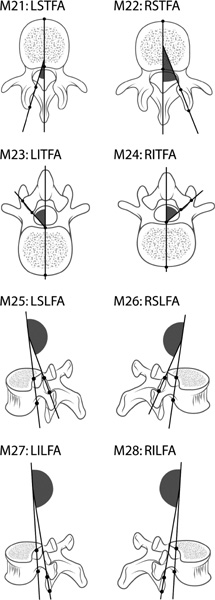
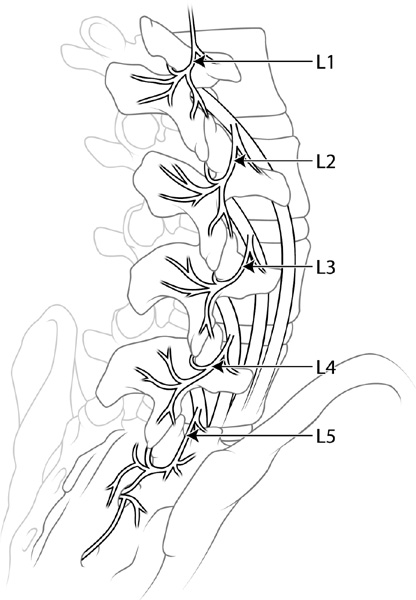
44 Motion-sparing or nonfusion technologies are becoming a part of the armamentarium of tools in the care of patients with degenerative disorders of the lumbar spine. Anterior nonfusion devices include total disk arthroplasty and nucleus pulposus replacements. Posterior nonfusion devices currently consist of three categories of devices: interspinous process spacers, pedicle screw–based soft stabilization systems, and facet replacements. This chapter focuses on facet replacements. Devices intended to replace the function of the lumbar zygapophyseal or facet joints are still in the early stages of development. However, with the initial success of anterior total disk replacement devices, there has been much interest in the development of this technology. Potential indications for facet replacements include: (1) as a stand-alone device for treatment of facet-related low back pain (LBP); (2) as an adjunct to total disk replacement; and (3) as a posterior dynamic reconstruction device after wide decompression for lumbar spinal stenosis. The mobile spinal segment is composed of a three-“joint” complex, the intervertebral disk anteriorly and the paired zygapophyseal or facet joints posteriorly. The facet joints are true synovial joints with hyaline cartilage–bearing surfaces and synovial lining. The lumbar facet joints are oriented in an oblique plane with curved, saucer-shaped surfaces. On an axial view, the facet joints of the lower lumbar spine are medially angulated 30 to 40 degrees. On a sagittal view, the joints are angulated anteriorly 10 to 30 degrees (Fig. 44–1).1–3 The unique location and orientation of the facet joints contribute to segment stability in resisting rotation, extension, and anterior translation of the cephalad level.4 Although the disk is the principal stabilizer of the motion segment, the facets are responsible for approximately half of the segmental torsional stability.5 The two opposing articular surfaces serve a “blocking” function to limit the allowable extent of motion and serve a “guiding” function to control segmental kinematics.6 In a standing position, the lumbar facet joints accept 15% of the compressive force of the body weight while the disk carries the remainder. The facets bear relatively less weight in flexed positions and relatively more weight in extended positions.7 The relative load-bearing property of the facet joints increases with the progression of spinal segment degeneration.8 The facet joint capsule is capable of expressing high levels of inflammatory cytokines and pain-related neuropeptides.9,10 The pain response is believed to be carried by nociceptive nerve fibers from the medial branch of the dorsal ramus. Each facet joint receives dual innervation from the dorsal rami of the level above the joint and the level of the joint. For example, the L4–L5 facet joint is innerved by the L3 medial branch (which courses over the L4 transverse process and downward to the joint) and the L4 medial branch (which courses between the superior articular process of L5 and the transverse process of L5, and curves upward to reach the L4–L5 joint) (Fig. 44–2). The medial branch also innervates the interspinous ligament and the multifidus and interspinal muscles. In contrast, the posterior margin of the intervertebral disk, the posterior longitudinal ligament, and the dura are innervated by the sinu-vertebral nerve off the ventral primary ramus.11–16 LBP is a ubiquitous condition with an annual incidence of 5% and a lifetime prevalence of 60 to 90%.17 Despite the advances of modern medicine, the exact etiology of LBP is still poorly understood. The various anatomical candidates believed to contribute to LBP are the disk, annulus, facet joints, sacroiliac joints, ligaments, and muscles. Traditionally, the intervertebral disk had been considered the primary pathological structure. However, with advances in diagnostic injection techniques, the facet joints have received recent attention as a pain generator. Figure 44–1 The facet joints are oriented obliquely in the sagittal and coronal planes. On an axial view, the facet joints of the lower lumbar spine are medially angulated 30 to 40 degrees. On a sagittal view, the joints are angulated anteriorly 10 to 30 degrees. Although few clinicians doubt the potential of the facet joints to cause pain, the relative contribution of facet-related (facetogenic) pain to chronic LBP is debated. Pathological facet joints are believed to contribute to pain in 8 to 70% of patients with chronic LBP.18–22 This wide range results from the varied methods used to make the diagnosis of facetogenic pain. However, studies using more stringent diagnostic criteria have demonstrated that facet joints are the single or primary pain generator in 10% of LBP patients.19,23,24 Figure 44–2 The anatomy of lumbar facet innervation. Each facet joint receives dual innervation from the dorsal rami of the level above the joint and the level of the joint. For example, the L4–L5 facet joint is innerved by the L3 medial branch (which courses over the L4 transverse process and downward to the joint) and the L4 medial branch (which courses between the superior articular process of L5 and the transverse process of L5, and curves upward to reach the L4–L5 joint). A major difficulty in accurately diagnosing facetogenic pain stems from a lack of specific clinical features. Traditionally, facetogenic pain was felt to be elicited by lumbar extension and rotation, maneuvers that stress the facet joints.23,24 However, studies using diagnostic injections as a gold standard have found that these maneuvers are nonspecific and refute the ability of any history or physical exam findings to identify primary facetogenic LBP.25–27 Clinical findings are difficult to interpret because the facet joints do not function in isolation but act as part of the three-joint complex. Therefore, any movement that stresses the facet joints likely stresses multiple other structures, such as the disk and ligaments. Because patients with degenerated facet joints usually have degenerated disks as well, pain-eliciting maneuvers are entirely nonspecific.28,29 In addition to the nonspecific clinical findings, most studies also fail to find a correlation between any radiographic abnormalities and facetogenic pain. Imaging studies such as plain radiographs, computed tomography (CT), and magnetic resonance imaging (MRI) have very limited value in identifying the anatomical structure (s) responsible for LBP. This is due to the abundance of “abnormal” findings in asymptomatic patients.30 Most persons over the age of 20 show radiographic evidence of age-related morphological changes of the spine, which are not necessarily pathological or causative of patient symptoms. Of the various modalities, CT is the best imaging test to visualize facet arthrosis.29 However, CT evidence of facet degeneration is seen in more than half of asymptomatic patients over 40 years old.31 In addition, there is no correlation between abnormal CT or MRI and relief of LBP by facet injection.32,33 High-resolution single photon emission computed tomography (SPECT) shows promise in diagnosing facetogenic LBP. Focal facet uptake has been shown to correlate with pain relief from facet joint injections.34,35 Currently, the most effective means to identify patients with facetogenic LBP is via diagnostic facet injections. Significant relief of LBP with an intra-articular injection of a local anesthetic should indicate the facet as the source of pain. Most clinicians use fluoroscopic guidance to deliver a small volume (< 2 mL) of anesthetic into the joints after confirmation of the intra-articular location with radiopaque contrast. However, injection protocols vary considerably between published studies. Some authors consider a subjective 50% relief of pain as significant, whereas others use a subjective 80% relief as a cutoff. Protocols with a single anesthetic injection or a double anesthetic injection have also been used.36,37 In a double injection technique, two separate injections using two different local anesthetics with different durations of effect are used. A positive only occurs when the duration of the patient’s pain relief is concordant with the anesthetic used. Single-injection techniques have a false-negative rate of 38% when compared with double-injection techniques.38 To improve specificity, other authors advocate even more stringent criteria such as: triple injections, identification of a negative control level, provocation of familiar symptoms with facet capsule distention,39 and concordance of a facet joint injection with a medial ramus block.40 Due to the lack of a true gold standard to diagnose facetogenic LBP, the sensitivities and specificities of these various diagnostic injection protocols remain unknown. With such difficulty in diagnosing facetogenic LBP, treatment results are expectedly varied. In two randomized prospective trials, therapeutic intra-articular steroid injections failed to demonstrate any superiority in pain relief when compared with placebo.36,41 Percutaneous radiofrequency ablation of the nerve supply to the facet joints was shown to be effective in many uncontrolled observational studies.42–44 However, in a randomized, prospective trial, radiofrequency denervation failed to show any treatment effect when compared with sham therapy.45 A similar randomized, prospective trial did show a therapeutic effect of radiofrequency ablation, but the patient numbers were small and the effect was modest and short-lasting.37 Lumbar fusion has also been suggested to treat patients with presumed facetogenic LBP who respond favorably to facet injections.46 However, a retrospective comparison demonstrated that the results of fusion in such patients were no better than nonoperative treatment.47 The ineffectiveness of currently available treatments for facetogenic LBP creates great potential for novel therapeutic approaches and technologies. Unlike the injection and neurotomy treatments, facet replacements can permanently remove the pain-generating articulation and capsule of the facet joints. Unlike fusion, motion and normal kinematics of the joint may be preserved. When used as a stand-alone device to treat facetogenic LBP, the prosthesis does not need to be anchored through the pedicles. Any design that removes the pain-generating portions of the facet joints and allows the remaining bone to anchor the prosthesis for bony ingrowth may be sufficient. Such a surface replacement design spares the pedicles to be used as spinal anchors in case a salvage revision procedure is necessary.
Facet Replacement Technologies
 Facet Replacement as a Stand-Alone Device for Facet-Related Low Back Pain
Facet Replacement as a Stand-Alone Device for Facet-Related Low Back Pain
 Facet Replacement as an Adjunct to Total Disk Replacement
Facet Replacement as an Adjunct to Total Disk Replacement
 Facet Replacement for Posterior Dynamic Reconstruction after Wide Decompression
Facet Replacement for Posterior Dynamic Reconstruction after Wide Decompression
 Facet Replacements Currently in Development
Facet Replacements Currently in Development
Anatomy
Facet Replacement as a Stand-Alone Device for Facet-Related Low Back Pain
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 Anatomy
Anatomy Conclusions
Conclusions