(1)
University of Pittsburgh Medical Center, Pittsburgh, PA, USA
Electronic supplementary material
The online version of this chapter (doi:10.1007/978-3-662-46976-7_6) contains supplementary material, which is available to authorized users.
6.1 Background
After massive weight loss (MWL), most patients seeking body contouring surgery, especially the older ones, dislike the sagging skin of their face and neck. Some simply inquire, but for others, facelift is a priority among many operations. When total rehabilitation from skin laxity is desired, staging and finances are major issues. That often means that the facelift is piggybacked during second or third stage of body contouring surgery. The challenge is to analyze the facial and neck changes and execute a cost-effective plan. For comprehensive management of the body contouring patient, skill in facelift surgery is an advantage.
Aging and environment cause atrophy of the skin, adipose, fascia, and bones. Longevity, chronic disease, poor nutrition, sunlight, emotional stress, and smoking are progressive and permanent insults to a youthful face. On the other hand, facial sag after MWL is primarily due to adipose deflation compounded by gravitational descent. In young MWL patients with good skin elasticity, liposuction and augmentation (Coleman 1997) are important. In middle-aged MWL patients with good-quality skin and subcutaneous fascia, their long-term response to a well-performed facelift surgery is excellent.
MWL patients in their mid-forties and beyond progressively show classic changes, sagging jowls, poor jawline definition, and loose skin of the upper neck (Ellenbogen and Karlin 1980). Through incisions about the scalp and ear, the adherent skin of the lateral face and mastoid is released in order to mobilize the midface, lower face, and neck (Mustoe et al. 2011). A vertical lift to the subcutaneous fascia is the optimal antigravity vector to improve the lower face (Tonnard et al. 2002). After superficial fascial suture suspension (Mitz and Peyronie 1976) of the face, excess skin is removed along the temporal scalp and in front of the ear. The greater the tissue laxity, the greater is the amount of skin resection. Even then, patients need to be cautioned that pleasing early results may sag within a year due to poor post MWL tissue quality that cannot be predicted. The younger the patient, the longer lasting is the facelift. Excess fat in the neck is removed directly or through syringe liposuction. Facial fat atrophy maybe reversed by lipoaugmentation primarily in the cheeks and perioral region. While upper neck skin laxity will be reduced with the vertical facial pull, a complete correction includes strong oblique lateral pull of the platysma and mastoid skin. Thorough syringe liposuction of the submental region is performed through the lateral neck exposure. Six to twenty ml of usable fat for facial augmentation can be harvested. Medial platysma bands are pulled laterally (Mustoe et al. 2011) with low transverse transection of prominent medial muscle bands. Direct submental platysma plication is rarely indicated. Patients obsessed with their platysma bands accept the risk of prolonged postoperative swelling and induration after extensive submental surgery.
Two types of vertical lifts are being performed to meet the challenge of effective, efficient, and naturally appearing face and neck rejuvenation. The short temple incision vertical facelift corrects lateral facial flattening, indistinct jawline, hanging jowls, and sagging upper neck. The extended vertical lift lengthens the incision across the entire temple into the lateral forehead. That extension to the lateral forehead allows a temporal, lateral canthal and malar dissection that elevates the mid cheek, smoothes out lateral facial and lateral canthal wrinkles, and raises the lateral brow.
6.2 Vertical Facelift
An effective and low-risk vertical facelift operation, taking about two and half hours, meets the challenge of efficacy and affordability in this surgically needy population. When the facelift is performed under surgeon-directed local anesthesia without an endotracheal tube and anesthesiologist, so much the better (Fig. 6.1, upper). There are no tubes, taping, drapes, poles, and IVs to navigate around the patient’s face. The face can easily be moved into any position comfortable to both the surgeon and the patient. Throughout the operation, there is an unobstructed view of the evolving results (Fig. 6.1, lower). Actually, this reduced cost-operative approach has worked out so well for massive weight loss patients that it has been adapted to most all aging faces.


Fig. 6.1
Case 6.1 Right anterior oblique intraoperative views immediately before and after a vertical facelift with lipoaugmentation of the cheeks and jawline. (Upper) With the unoperated head reclined, the sagging midface and jowl fall back to dense retinacular subdermal network along the lateral face. Except for the lateral canthal region, this dam to the flow of the midface corresponds to the anterior extent of dissection as marked with dash line. (Lower) The dam adherence to the midface has been surgically disrupted, allowing an effective vertical skin pull. Under the redraped skin the lateral face is filled by imbricated SMAS and thick skin flaps. The matching medial face is filled with injected fat from the abdomen
The vertical lift is often combined with submental liposuction and midface lipoaugmentation. The routine operation, adaptable to a variety of presentations, is a moderately extensive sharp lateral face subcutaneous undermining followed by a forceful vertical SMAS and oblique platysma suture ten-step imbrication using double-armed barbed sutures (Fig. 6.2). With sequential cinching, the SMAS is progressively lifted (Fig. 6.3). The vertical fascial skin pull transfers most of the excess lower facial and upper neck skin to the temporal hairline with only a narrow excision undulating in front of the ear (Fig. 6.4). The 3–4 cm-wide temple transverse band skin excision makes a hair-bearing scalp resection for a hidden scar unrealistic, except for exceptionally low-lying hairlines. A single-layer running closure gathers the longer facial skin flap along the temporal hairline incision (Fig. 6.5). Obliquely pulled neck skin requires a postauricular and mastoid hairline closure (Fig. 6.1, lower). Lipoaugmentation of the planned areas by Coleman cannulas through 18-gauge needle sticks from harvested abdominal fat completes the facial rejuvenation (Coleman 1997).
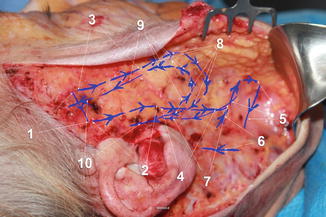
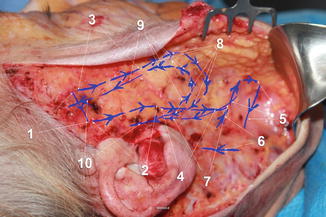
Fig. 6.2
Case 6.1 The right side of the face superficial fascia and platysma muscle are exposed for #1 PDO Quill suture imbrication. An overlay of the 1 through 10 stepwise imbrication pattern is drawn with arrowheads indicative of the direction of the suturing and angle of the barbs
Fig. 6.3
Case 6.1 Start of imbrication of the SMAS with 36 mm. ½ circle taper needle, double-armed 48 cm long barbed suture. (Left) A rake retractor holds the thick skin flap. Little adipose lies on the SMAS. The first bite is through all layers of temporal fascia superior to the zygomatic arch and anterior to auricular temporal neurovasculature. Without a knot to tie, the suture need not be buried. (Right) After two descending bites (as indicated in Fig. 6.2, 1 and 2), the ends are pulled superiorly to cinch narrow rolls in the SMAS. Both the jowls and upper neck skin are nearly fully suspended
Fig. 6.4
Case 6.1 Planning the right facial skin excision. (Upper) Following suture suspension of the SMAS, the facial skin flap is pulled superiorly for marking the excision along the temporal and preauricular incisions. (Lower) The marked skin is draped across the face, prior to being excised
Fig. 6.5
Case 6.1 Excision and closure of excess facial skin. (Upper) The temporal and preauricular skin excess has been excised along the markings with the hatch marked skin overlapping the tragus to be sutured to the temporal helical junction. (Lower) Starting at the forehead, the longer facial skin flap is suture advanced to accommodate the temporal incision line, leaving small rolls that smooth out over months
6.2.1 Case 6.1 Vertical Facelift in a Thin-Weight-Loss Patient
Case 6.1 is a detailed presentation of the common vertical facelift. The preoperative marked images for the intraoperative sequence just presented belong to a 5′ 4″, 65-year-old MWL woman (Fig. 6.6). After her gastric bypass, her weight went from 231 lb to 115. Her midface is hypoplastic with skin hanging over her jawline. Her sweeping skin laxity of the neck is greatest at the submental region. The markings plan an oblique temple-long incision to the superior helix, then posterior to the tragus, and around the earlobe. Unseen is the continuation along the auricular-mastoid sulcus. It is then visualized descending along the mastoid hairline. The extent of undermining of the lateral face is indicated by the dashes that start at the anterior aspect of the temporal incision to descend posterior to the lateral canthus and jowls to the lower neck. The mid cheek as well as the perioral and pre-jowl sulcus are marked for lipoaugmentation while simulating the anticipated facelift. The fat grafting will be performed through percutaneous Coleman blunt needle injections immediately following the facelift. Processed fat from the abdomen is injected, 8 cc in each cheek, 4 cc in each jowl, and 4 cc in the lips. The critical aspects of the operation are seen in Figs. 6.1, 6.2, 6.3, 6.4, and 6.5.


Fig. 6.6
Case 6.1 A thin, aged massive weight loss patient is marked for a vertical facelift. (Left) Frontal face markings visible for liposuction of submental region and lipoaugmentation of the lips and junction between the chin and jawline and her mid cheeks. (Middle) Right anterior oblique markings show profound ptosis of her mid cheeks and jowls. The facelift incision hugs the temporal hairline. (Right) The extent of skin submental skin laxity is evident as well as the entire planned incision
The result 1 year later demonstrates synergy of an effective facelift with localized lipoaugmentation (Fig. 6.7). The considerable excess skin of the neck has been removed. The long suture line courses inconspicuously along the temple hairline, post tragal, and behind the ear and along the short mastoid skin closure. There are no oblique ridges. She has a natural, younger appearance with no hanging skin or wrinkles. The tragus and earlobe positions are natural. Imbrication of the lateral SMAS under a thick skin flap left a youthful transition from her mid to lateral face. She looks as she did 20 years earlier (Fig. 6.8). This youthful sculpture is dramatically visualized through comparative 3-D image scanning, using Axis Three (Fig. 6.9). Her facial wrinkles are effaced as her midface subtly tapers into the lateral face. There is an edgewise obliquely viewed ogee curve.



Fig. 6.7
Case 6.1 One year following the vertical facelift and lipoaugmentation. The sagging facial and neck skin have been pulled back. The jawline is smooth. The mid cheeks are raised and full. There is youthful tapering from mid cheek to lateral face

Fig. 6.8
Case 6.1 A natural facial rejuvenation. (Left) Facial photograph taken 21 years ago, shortly before a rhinoplasty. (Right) A similar pose for a photo taken 1 year after her facelift. Her nose is shorten and tip narrower and her eyebrows higher. Otherwise, a 20-year restoration has occurred
Fig. 6.9
Case 6.1 Pre- and 1-year postoperative 3D facial scan shows one of an infinite number of images. Her mid and lateral facial wrinkles have smoothed, whereas the wrinkles on the unoperated forehead remain unchanged. The submalar transition across the mid and lateral face is youthful
Immediately preoperative, she is comfortably reclined and adequately sedated with 2 mg of Ativan (Fig. 6.1, upper). In this position, her mid cheek, jowls, and submental contours are normal. Densely distributed subdermal retinacular ligaments posterior to the dashed line inhibit posterior sag over the ears. A slight anterior and inferior drag of the cheek restores the aged anatomy. Her considerable mid cheek and lower facial skin laxity translates into a wide band of removal through the temple, so much so that the attempt to preserve her low sideburn, leaving the posterior part of the excision within her temple scalp, proved futile.
Following blocks of the great auricular and auriculotemporal nerves, relatively dilute local anesthetic with epinephrine slowly hydrodissects the supra SMAS and platysma planes. This technique is nearly painless and facilitates later swift scalpel dissection. The right-side incision cuts perpendicular along the temporal hairline and continues through the temple, staying superficial to the temporoparietal fascia and then around the ear to end at the mastoid cervical junction. Scalpel dissection raises a thick skin flap off superficial fascia through platysma. Then facelift scissors complete the skin flap elevation about the dashed line. Undermining superficial to the easily identifiable lateral orbicularis and levator muscles is safely superficial to branching facial nerve. Not only does this thick skin flap dissection retain vascularity, but also the subsequent SMAS and platysma imbrication is unencumbered by adipose. Hemostasis is by pinpoint electrosurgical bipolar coagulation.
The #1 PDO Quill suture imbrications of the SMAS and platysma is drawn and labeled 1 through 10 steps on the dissected SMAS/platysma field as modified from the MACS operation (Fig. 6.2). For cost savings, only a single suture is used on each side of the face. After single deep temporalis fascia fixation bite (1) from one of the two 32 mm long Quill taper needles, each needle takes descending and slightly divergent two SMAS skimming bites (2, 3




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree