, Madan Ethunandan2 and Tian Ee Seah3
(1)
Poole Hospital NHS Foundation Trust, Poole, Dorset, UK
(2)
Department of Oral and Maxillofacial Surgery, University Hospital Southampton NHS Trust Southampton General Hospital, Southampton, UK
(3)
Orange Aesthetics and Oral Maxillofacial Surgery, Singapore, Singapore
Subunits and Anatomical Considerations
Eyelids perform many important functions, which include protection of the eye and maintaining an adequate tear film. The aesthetic eyelid unit is defined by the lower margin of the eyebrow, the lateral and inferior orbital rims and the nasojugal fold. A sound understanding of anatomy and function is essential for eyelid reconstruction and should only be attempted by an appropriately trained clinician.
The eyelids are complex multilayered structures supported by cartilaginous tarsal plates. The free lid margin contains eyelashes and secretory glands and the extension of the tarsal plates forms the medial and lateral canthal tendons.
Reconstruction could be more easily understood if the eyelids were considered to consist of an anterior lamella composed of skin and orbicularis oculi and a posterior lamella composed of the conjunctiva, tarsal plate, orbital septum and lid retractors. The tarsal plate and orbital septum together is sometimes considered as the middle lamella. The “grey line” along the lid margin represents the junction between the anterior and posterior lamellae.
The eyelid aesthetic unit can be further subdivided from a reconstructive point of view into the upper lid, lower lid, medial canthus and lateral canthus subunits (Fig. 8.1).

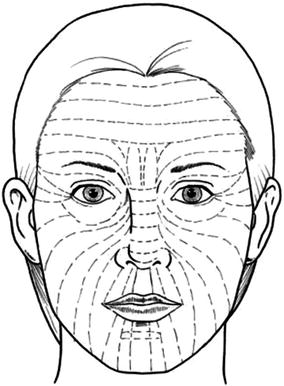

Fig. 8.1
Eyelid subunits
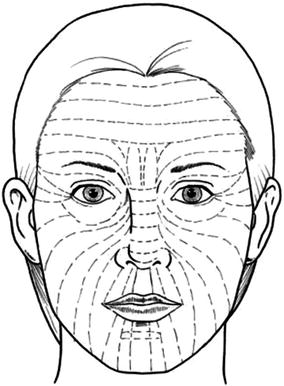
Fig. 8.2
Orientation of RSTL’s
The skin of the eyelid is the thinnest in the body and the RSTLs around the eyelids are horizontally oriented (Fig. 8.2). However, excision parallel to the RSTLs, especially in the lower eyelid, runs the risk of eyelid retraction and ectropion. It is therefore preferable to orient excisions to be perpendicular to the lid margins, unless there is significant skin redundancy. Excisions along the RSTL in the adjacent lateral and medial canthus, eyebrow and glabellar regions can be performed and will provide relatively unobtrusive scars.
Full-thickness defects require reconstruction of both the anterior and posterior lamella, in which case it is mandatory that at least one of the reconstructed lamella should contain its own blood supply.
Upper Eyelid
Anterior Lamella Defects
Primary Closure
Indications
Small defects
Technique
The defect is modified into an ellipse with a vertical orientation. The wound margins are undermined and the defect closed in layers.
Tips
In patients with eyelid skin redundancy, horizontal ellipse along the RSTLs could be undertaken, taking care to avoid ectropion.
Advancement Flap
Indications
Medium defects
Technique
The defect is modified to obtain parallel wound margins. Incisions are made from the extremity of the defect and the flap raised in the sub-muscular plane. The wound margins are undermined and the defect closed in layers (Fig. 8.3a–c).
Tips
The base of the flap can be made broader to maintain a satisfactory vascular pedicle. The flaps can be medially or laterally based but when based medially, should not extend beyond the confines of the eyelid skin.
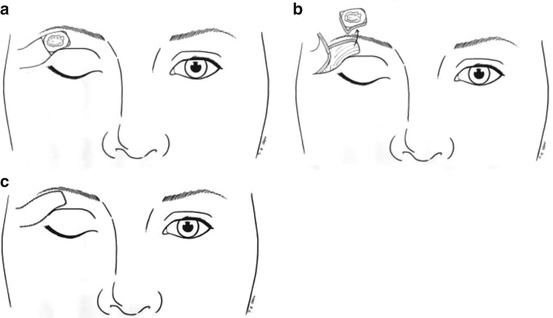
Fig. 8.3
Advancement flap
Fricke Flap
Indications
Medium and large defects (upper and lower eyelid)
Technique
It is an inferiorly based transposition flap harvested from the temple/forehead skin situated lateral and superior to the orbit/eyebrow. The margins of the defect are delineated and the flap designed with its inferior medial margin lying along the lateral margin of the defect. A trial transfer is carried out to determine the length of the flap and should take into account loss of length due to rotation around the pivot point. The flap is raised in the subcutaneous plane and transposed into the defect. The donor site defect is closed initially followed by insetting the flap into the defect (Fig. 8.4a–d).
Tips
The length to width ratio should not exceed 4:1 to maintain adequate vascularity. The medial extent of the flap should stop short of the supraorbital neurovascular bundle. Care should be taken to avoid damage to the branches of the facial nerve, which lie on the deep surface of the muscles. Thinning of the flap might have to be undertaken, either during the initial transfer or at a later stage.
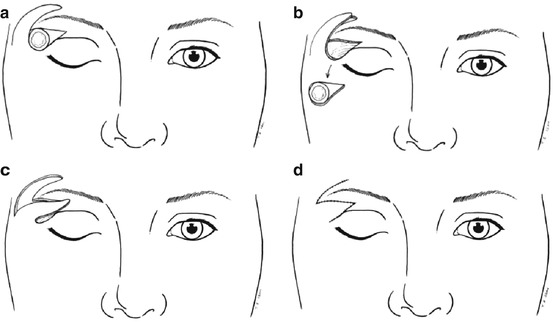
Fig. 8.4
Fricke flap
Glabellar Island Flap
Indications
Medium defect (medial canthus, medial upper eyelid)
Technique
An accurate template is made of the defect and marked out at the donor site along the horizontal glabellar skin crease. The skin is incised all around the flap up to the subcutaneous tissue. The incision along the superior margin of the flap is deepened down to the periosteum and the skin medial to the defect and inferior to the proposed flap is raised in the subcutaneous plane. The flap pedicle consisting of subcutaneous tissue and muscle is gradually released in the supra-periosteal plane, to obtain the required mobility. The flap can be rotated upto 120 degrees. The mobilised flap is sutured into the defect and the donor site closed primarily, following undermining of the wound edges (Fig. 8.5a–e).
Tips
The thickness of the subcutaneous pedicle can alter the contour of the medial canthus region and can be corrected at the second stage if required. Consideration should be given to extending the elliptical skin incision to the contra-lateral medial brow to obtain a symmetrical glabellar skin crease and elevating the nasal tip. Care should be taken to avoid damage to the pedicle during dissection and haemostasis.
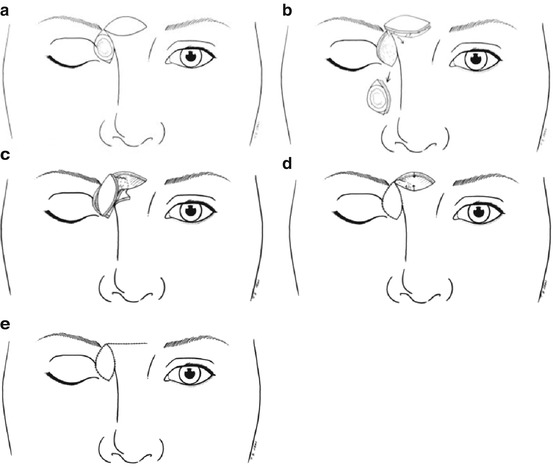
Fig. 8.5
Glabellar island flap
Full-Thickness Defects
Primary Closure (See section “Lower eyelid” – Fig. 8.8a–d)
Indications
Small defects
Technique
The lesion is excised to leave a shield-shaped defect, with parallel sides towards the lid margin. The wound is closed in layers with sutures placed in the tarsal plate, avoiding going through the palpebral conjunctiva. The orbicularis oculi and skin layers are then closed.
Tips
Accurate approximation of the lid margin is essential to prevent notching and can be helped with vertical mattress sutures along the grey line. It is often helpful to place all the sutures in the tarsal plate, prior to tightening.
Primary Closure with Lateral Canthotomy and Cantholysis (See section “Lower eyelid” – Fig. 8.9a–e)
Indications
Medium defect
Technique
The lesion is excised to leave a shield-shaped defect. A 1 cm incision is made through the skin and orbicularis muscle overlying the lateral canthus. The lateral canthus is next divided (canthotomy) horizontally between the upper and lower limbs, up to the bony orbital rim. The upper lid is put under tension and the superior limb of the lateral canthus transected (cantholysis) vertically, till it is completely released from its lateral attachments. The primary defect is closed in layers followed by the skin incision overlying the lateral canthus.









