CHAPTER 37 Extended Trochanteric Osteotomy
Posterior Approach
KEY POINTS
 Consider an extended trochanteric osteotomy for the removal of well-fixed implants, for the removal of retained distal cement, and for patients demonstrating varus femoral remodeling.
Consider an extended trochanteric osteotomy for the removal of well-fixed implants, for the removal of retained distal cement, and for patients demonstrating varus femoral remodeling. The length of the extended trochanteric osteotomy should be minimized to use the shortest femoral revision stem possible yet should be long enough to bypass the apex of the femoral remodeling, to achieve component and cement removal, and to allow at least two cerclage cables to be placed around the osteotomy.
The length of the extended trochanteric osteotomy should be minimized to use the shortest femoral revision stem possible yet should be long enough to bypass the apex of the femoral remodeling, to achieve component and cement removal, and to allow at least two cerclage cables to be placed around the osteotomy. When levering the osteotomy anteriorly, multiple wide osteotomes should be used simultaneously to distribute the stress along the greatest distance.
When levering the osteotomy anteriorly, multiple wide osteotomes should be used simultaneously to distribute the stress along the greatest distance. A prophylactic cerclage can be placed distal to the osteotomy before femoral preparation and stem insertion to minimize the risk of fracture.
A prophylactic cerclage can be placed distal to the osteotomy before femoral preparation and stem insertion to minimize the risk of fracture.INDICATIONS
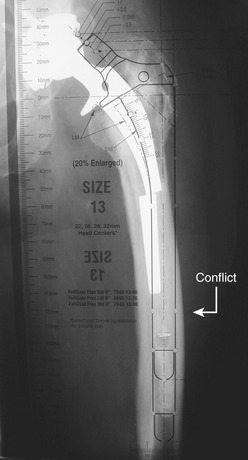
The most common indications for the use of an extended trochanteric osteotomy include removal of a well-fixed femoral implant; removal of retained distal cement; insertion of a femoral component in patients with proximal femoral remodeling; and improved surgical exposure (Fig. 37-1).