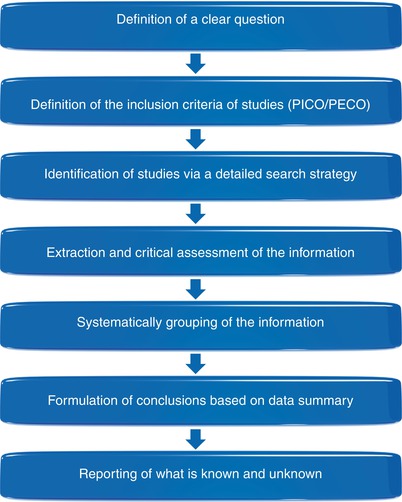
Fig. 1.1
Evidence-based dentistry (EBD) diagram “for periodontal plastic surgery (PPS)”
One of the most important characteristics of evidence-based decision-making regards to the translation of the results of research to conventional clinical practice. Apparently, this does not seem to represent a difficult task; however, it is dependent of a critical appraisal of what different (many times a bunch of) studies have identified as clinically relevant for use and the meticulous handling of these information.
An “evidence-based periodontology” now concentrates its efforts in asking about the known and unknown information of interest, finding and appraising the best sources of evidence and examining and adjusting such outcomes for clinical practice in order to provide the best treatment options to patients’ needs [10]. The main tools used to achieve such purpose (systematic reviews [SR] and meta-analysis studies) have been growing in popularity because they may provide standardized, precise, consistent and qualified data combination of several quality-assured individual studies [1]. For instance, clinicians may search for the evidence in case reports, case series and randomized clinical trials and arbitrarily give the same “weight” (relevance) to them all (Fig. 1.2). The purpose of an evidence-based decision-making is to truly provide the directions to be followed when considering different options of treatment by allowing the clinicians to draw trustworthy conclusions based on the “scientific truth” and the ways to apply it in their practices [1, 3].
Fig. 1.2
Level of validity and confidence of outcomes according to study type [1]
Based on that, “evidence-based periodontal plastic surgery” was defined as “the systematic assessment of clinically relevant scientific evidence designed to explore the aesthetic and functional effects of treatment of defects of the gingiva, alveolar mucosa and bone, based on clinician’s knowledge and patient-centred outcomes, such as perception of aesthetic conditions, functional limitations, discomfort, root sensitivity, level of sociability after surgery and preferences” [8–11]. Consequently, the primary argument to creating a background to judge and improve the quality of treatment with periodontal and peri-implant plastic surgery procedures should be the identification of the appropriate base of evidence for each respective therapy.
1.2 Evidence-Based Decision-Making: “Why Should I Base My Treatment Plan on Evidence-Based Clinical Approaches?”
The implication of truly basing a treatment plan on evidence-based clinical approaches for health promotion relies in the use of a structured sequence of criteria in the retrieval and extraction of the best source of information available for a condition or disease [10]. These steps regularly followed by high-quality systematic reviews (SRs) and overviews (i.e. reviews of SRs) undoubtedly search to convert the information of efficacy research to clinical effectiveness; that is the translation of the results achieved at university research to conventional daily practice.
It is important to consider that SRs are planned to recognize, appraise and combine information from clinical trials to provide evidence-based responses and alternatives to clinical research problems [1, 3–11]. Queries linked to development of the clinical decision-making process, estimation of the value of treatment modalities and assessment of disparities in daily practice motivate clinicians to “read” an SR. Thus, these issues can provide important scientific basis of information for clinicians since they identify current knowledge (i.e. what is known and unknown) [1, 3–11].
On the other hand, some obstacles related to the best ways of interpreting the findings of these review studies may be transposed. Most of the clinicians are not trained on how to critically manage the group of findings of an SR neither to identify the central points that could not have been adequately reported in the publication. Consequently, a noticeable difficulty in interpreting their outcomes strengthens the condition that an SR has to report as maximum as possible (and in a transparent manner) the main criteria employed in the preparation of its research protocol. As such, it will provide the clinicians and experts that will read it the capacity to understand and distinguish what has been reported [1]. Based on that, the translation of research findings to clinical practice (by the critical assessment of the evidence available) will be able to guide the decision-making process.
1.3 Systematic Reviews: “Why Are They Useful?” and “Should They Limit My Practice?”
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree