Fig. 2.1
Radiograph of a pelvis in a spinal cord injured patient showing severe lumbo-thoracic spine deformity

Fig. 2.2
Radiograph of a pelvis in a spinal cord injured patient showing dislocated left hip joint
2.4 Severe Muscle Spasms
Severe muscle spasms are seen in spinal cord injured patients or those with advanced neurological diseases. Individuals with this condition cannot lay down or sit in a proper pressure relief position, which leads to development of pressure ulcers. Severe muscle spasms can create shearing forces between the skin and the underlying sheets or cushion. This can cause extensive ulcerations over the heels or ulcerations between the medial surfaces of each knee. Severe spasms of the hip flexor can cause hip subluxation or dislocation and consequently cause ulceration over the boney prominence (e.g., the greater trochanter). Contracture of the flexor muscles and the adductor muscles of the hip joint and the hamstring muscle of the posterior thigh resulting from the spinal injury or neurological disease secondary to neurological imbalance of the muscles function cause severe spasticity. Contractures predispose to developing pressure ulcers by preventing the individual from sitting or lying in a normal functional position where pressure will be distributed evenly. Consequently, part of the pelvis will experience higher pressure than other areas, eventually leading to skin breakdown. In addition, the contracture results in difficulty in performing hygienic care to the groin and inner thigh area, which can lead to fungal infection of the skin.
2.5 Other Factors Contributing to the Development of Pressure Ulcers
Medical conditions that can break or weaken the integrity of the skin, for example, skin allergic disease from medications that are applied locally and can cause reaction in the skin. This inflammation or breaking in the skin will be a nidus for developing pressure ulcers. External materials applied on the skin, for example, dressing tapes that can cause blisters and cast applications in insensate or geriatric patients without protective padding, will cause pressure ulcers especially over the heels, shin, patella, and both malleolar at the ankle site. Careful attention should be paid when a cast is required in this insensate group of patients. Tight elastic pressure bandages can cause the same effect on the skin, resulting in blisters and stage II or III ulcers.
Patients with immune-compromised syndromes like HIV and those on systemic medications like steroids can experience changes in the skin. This can predispose the skin to break down easily. Patients who smoke or abuse drugs [16, 17] have a higher incidence of pressure ulcer than nonsmokers [18–20] as a result of the pharmacological effect of nicotine that impairs blood circulation.
Quadriplegic patients are at a higher risk of developing pressure ulcers than paraplegic patients. Development of any acute illness in a quadriplegic patient (e.g., pneumonia, urinary tract infection) will confine the patient to bed, whether at home or in hospital, and eventually leads to development of pressure ulcer. This condition is most commonly seen when a history is taken from the quadriplegic patient post pressure ulcer development. A premorbid psychosocial condition existing prior to spinal injury is a factor in development of pressure ulcers in this group of patients.
2.6 Site of Pressure Ulcer Development
High-risk patients commonly develop a pressure ulcer when laying down without movement, for example, in the supine position secondary to illness, injury, or during surgery on the operating table, or even during special radiological procedures. The most common sites where pressure ulcers develop are the bony prominence, of the body, such as the occipital area, the scapular ridge, the spinous process, the sacrococcygeal area, and the calcaneus bone. If the patient is placed on their side, that is, the lateral position, the trochanteric area is subject to pressure and consequently develops skin breakdown. Remaining in the sitting position for prolonged periods of time without a proper cushion or pressure relief causes ischial ulceration, in addition to the predisposing factors existing in this group of patients.
In spinal cord injured patients, the circumstances regarding the site for development of pressure ulcers differs somewhat because, in the acute injury phase, there are common sites, and there are other sites in the post-recovery phase and rehabilitation with integration back into normal daily life in society.
A study by the model system of spinal cord injury patient care in the United States [21] found that during early treatment in the acute phase of the spinal cord injury at trauma centers, for stabilization of the spinal shock and the spine, patients were kept in the supine position in bed for numerous medical reasons. The findings for the common ulcer site areas were occipital = 2.6 %, scapular = 4.3 %, spinous process = 1.3 %, iliac crest = 1.8 %, sacrum = 37.4 %, trochanteric = 3.8 %, ischium = 9.2 %, elbow = 2.0 %, knee = 1.5 %, and malleolar = 3 %. The anatomical distribution of the ulcer sites somewhat changed when patients were followed in the first year post injury, when the common sites were the sacrum = 20 %, ischium = 18.3 %, trochanteric = 12.4 %, heel = 16.6 %, elbow = 2.6 %, and malleolar 8.7 %. The reasons for the ulcer distribution at this phase of a patient’s life were sitting in a wheelchair and resuming normal life without practicing pressure relief as instructed in rehabilitation post injury. Laying down in bed in the supine position or lateral position without a pressure relief mattress can predispose to ulcer development in the sacrococcygeal area and trochanteric area.
2.7 Local Pathological Changes and Sequel in Pressure Ulcer Stage IV
Pressure ulcers in different parts of the body frequently progress with local pathological changes and manifest clinically with a different appearance than simple stage IV ulcer. This presents a difficult diagnosis because of the pathological changes of the ulcer, even with the utilization of advance diagnostic modalities, and it thus presents a clinical dilemma to the surgeon and infectious disease specialist. On many occasions, the diagnosis of complex pathological changes is discovered accidentally during surgery for ulcer closure or debridement. Therefore, the pathological changes lead to modifications in the management plan for the ulcer. Clinical exposure and experience with clinical thinking and taking into account these changes is important for the practicing specialist dealing with these complex, difficult wounds. In the following section, the pathological changes in each anatomical ulcer location are discussed in details.
2.8 Sacrococcygeal Ulcer
Extensive necrosis and infection of the skin and the subcutaneous tissue leads to necrosis of the pre-sacral fascia, which covers the sacrum and the coccygeal segment, considering the anatomical fact that gluteus maximus muscle does not cover this area (Fig. 2.3).


Fig. 2.3
Showing extensive necrosis of the pre sacral fascia and ligament
If a pressure condition continues in this area, ischemia and necrosis extend to involve the gluteus maximus muscle, which physiologically is more sensitive to ischemia than other tissues. Consequently, necrosis will occur in the muscle fibers. This condition is difficult to detect if only part of the muscle is exposed; otherwise, it may be discovered accidentally during surgery. The macroscopical pathological appearance of the muscle is “dull gray” color in appearance. Incising the affected muscle demonstrates no bleeding, and the muscle does not contract with electrocautery touch. Debridement should be done to all the necrotic muscle parts, which eventually leads to a small volume of muscle. A sample of the muscle should be sent for anaerobic bacterial culture and sensitivity. The wound should be irrigated with a high-pressure irrigation system in the operating room. Wounds in this condition cannot be closed in one stage and should be closed in two stages to avoid flap complications. Other manifestations of the sacral wound are the formation of abscesses that result in pus formation between the gluteus maximus muscle and gluteus medius muscle (Fig. 2.4). Also, infection and necrosis can extend to the sacrotuberous ligament. Eventually, communication can occur between the sacrococcygeal ulcer and ischial area with involvement of the ischiorectal fossa, which consists of fibro-fatty tissue. Dissection of the infection can extend around the anal canal. A diverting colostomy is necessary in these conditions (Fig. 2.5).


Fig. 2.4
Involvement of the gluteus maximus (G.M.) with sacrococcygeal ulcer
Fig. 2.5
Connection between the sacrococcygeal ulcer and ischial ulcer
2.9 Ischial Ulcer
Ischial ulcers can extend into the perineum in the male patients. This pathological change is seen more frequently than in female patients because of the existence in males of soft tissue space between the anus and the scrotal sac. The result is the involvement of the deep tissue, which includes the perineal urethra. Clinically, urine will be seen leaking from the ischial ulcer (Fig. 2.6). To confirm the clinical diagnosis, a urethra cystogram study using radio-opaque dye and x-ray will confirm the extravasation of the urine outside the perineal urethra. In this condition, temporary diversion of the urine should be accomplished by suprapubic cystostomy or permanent urinary diversion in recurrent conditions. This allows the surgical repair of the involved urethra during the flap closure of the ulcer (Chap. 8).


Fig. 2.6
Involvement of the perennial urethra by ischial ulcer extension and necrosis
Another important pathological condition that can occur, especially in spinal cord injured insensate patient with diabetes, is Fournier’s gangrene of the scrotum and perineum secondary to descending infection from ischial ulcer. This type of infection caused by a gas-forming organism (anaerobic) infection. This serious condition requires urgent decompression and debridement, and, later, reconstructive surgery (Figs. 2.7, 2.8, 2.9, and 2.10).

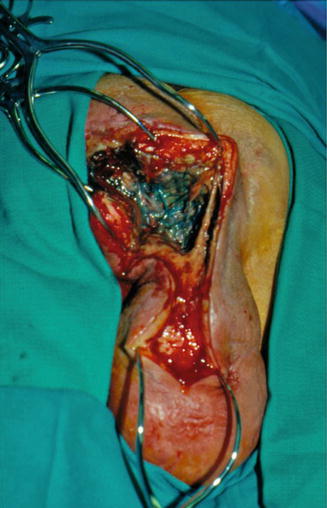





Fig. 2.7
Swelling of the scrotum secondary to descending infection from the ischial ulcer, Q-tip demonstrating the connection with the scrotal sac
Fig. 2.8
Plain x-ray of the scrotal area showing gas bubble secondary to gas forming organism
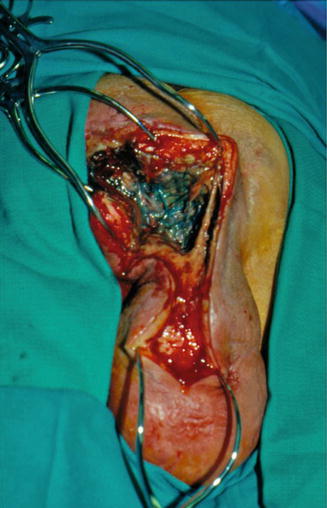
Fig. 2.9
Operative photograph showing the debridement and decompression of the scrotal sac
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree