(1)
Department of Dermatology, Drexel University, Philadelphia, Pennsylvania, USA
Abstract
This work has been devoted to the concept that atopic dermatitis is initiated by biofilm-producing staphylococcal bacteria. In a brief précis of psoriasis, we marshal the evidence that psoriasis is initiated by the bacterium Streptococcus pyogenes. While we fully believe these diseases are provoked by these two specific bacteria, we do not believe that either of these diseases is an infection. In eczema, it is the production and location of the biofilms (made by staphylococcal bacteria) in eccrine ducts that we believe is crucial. In psoriasis, we believe it is an immune reaction to the streptococcal bacteria that is likewise crucial.
Keywords
EczemaMyD8PAR2Protease-activating receptor 2Psoriasis Streptococcus pyogenes Toll-like receptor 2Tumor necrosis factor αThis entire work has been devoted to the concept that atopic dermatitis is initiated by biofilm-producing staphylococcal bacteria. In a brief précis of psoriasis, we will marshal the evidence that psoriasis is initiated by the bacterium Streptococcus pyogenes. While we fully believe these diseases are provoked by these two specific bacteria, we do not believe that either of these diseases is an infection. Even if humanely possible, Koch’s postulates (which help define an infection) could not possibly apply to either disease. The postulates state that (1) bacteria should be found in all people with disease; (2) the bacteria should be isolated from lesions of infected persons; (3) a pure culture of the bacteria, inoculated into a susceptible host, should produce symptoms of the disease; and (4) the same bacteria should be reisolated from the intentionally infected individual. In eczema, it is the production and location of the biofilms (made by staphylococcal bacteria) in eccrine ducts that we believe is crucial. In psoriasis, we believe it is an immune reaction to the streptococcal bacteria that is likewise crucial. The mere presence of the organisms is only part of the story. In other words, it is not which bacterium is present, but what those bacteria are doing.
In eczema, we have found staphylococci on routine cultures from lesions. XTT assays from these bacteria show that they are multidrug resistant and the same XTT assays and the Congo red cultures show that they are capable of producing biofilms. Genetic analysis of these same bacteria shows them to have genes known to produce biofilms. We have also found occluded eccrine sweat ducts in lesional skin in this disease; these occlusions contain a periodic acid–Schiff (PAS)-positive material that we believe stains biofilm because it stains exopolysaccharides and the biofilms are composed mostly of polysaccharides. These occlusions also stain positively for Congo red, which stains for amyloid. This conclusively identifies those occlusions as biofilms, inasmuch as amyloid forms the infrastructure of biofilms and is found nowhere else in normal skin. We have recovered biofilms only from lesional skin, not from normal skin. The various staphylococci are present on lesional and normal skin because they are normal flora. Everyone has them.
On immunopathology of lesional skin in eczema, we have demonstrated Toll-like receptor 2 (TLR2) activity in the stratum corneum adjacent to the sweat duct occlusions. TLRs react against gram-positive bacteria in their role in the innate immune system. Where the biofilms are produced by gram-positive staphylococci, the location of the innate response periductally in the stratum corneum (where the occlusions caused by the biofilms are situated) is very strong presumptive evidence that they are stimulated by the sweat duct occlusions. In nonlesional skin, TLR2 activity is present in the basal zone of the epidermis and not in the stratum corneum.
TLR2 activity in its innate immune response stimulates known pathways to react against invading pathogens. Among these is the MyD88 pathway, which is triggered by this response. This pathway generates the molecule nuclear factor-κB (NF-κB), itself a particle generating many responses, among which is tumor necrosis factor α (TNFα). This latter is the most potent stimulant of spongiosis, the most common pathological finding in eczema. Another is the stimulation of protease-activating receptor 2 (PAR2), one of the most potent stimulators of itching known. Thus, the most important symptom and the most important pathologic finding can be readily accounted for by TLR2 stimulation. Both are activated through intermediaries: MyD88 adapter-like/TIRAP (TIR domain-containing adaptor protein) in the MyD88 pathway and (most likely) kallikrein in the PAR2 pathway. Both of these intermediaries are present in abundance proximal to the TLR2 activity.
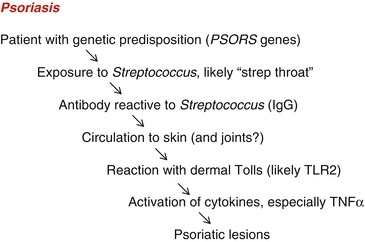
We further postulate that the story in atopic dermatitis is a double-hit phenomenon, with the bacterium playing the role of the environmental hit (Fig. 11.1). The filaggrin gene plays the important genetic role in most patients. The story in psoriasis is a similar double-hit phenomenon, with the genetic hit one of the PSORS genes. Evidence points to the PSORS2 gene as perhaps the most likely [1]. This gene is also most likely autosomal dominant, with variable penetrance. The environmental hit in psoriasis is S. pyogenes (Fig. 11.2).
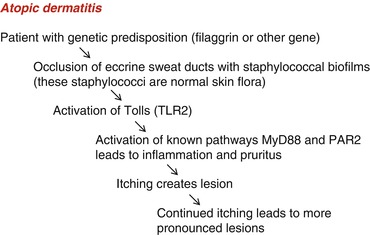
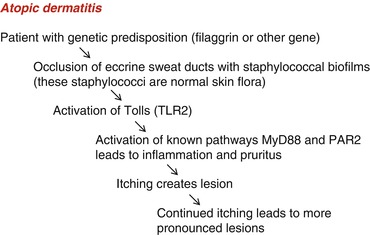
Fig. 11.1
Atopic dermatitis