Fig. 9.1
(a–c) Large squamous cell carcinoma on the scalp treated with electrons and bolus. Result 6 weeks after the end of the treatment
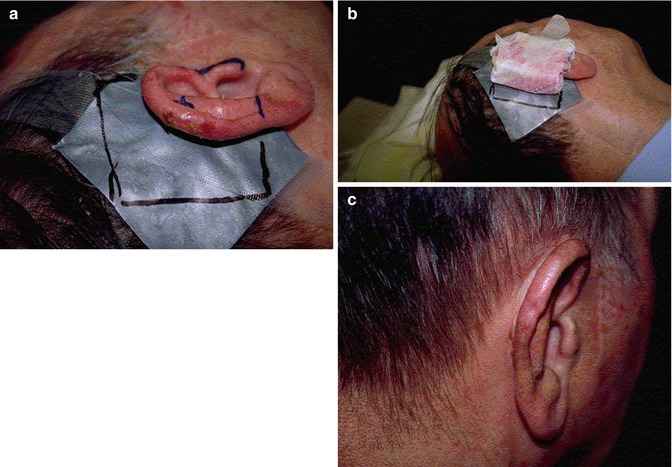
Fig. 9.2
(a–c) Basal cell carcinoma treated with electron beam. A wax mold is placed to diminish the dose inhomogeneity. Result 6 months later
9.2 Electron Beam Characteristics
Some characteristics of the electron beams make them interesting for the treatment of certain skin carcinomas, especially when their localization makes the surgery or the treatment by X-rays less relevant. Electron beams are characterized by a rapid isodose falloff at depth below the skin surface, which means that there is little or no radiation exposure beyond a defined depth. The range of the depth to be irradiated is controlled by the selection of the appropriate energy. Although differences in body densities represent important inhomogeneities for electrons, the additional problem of strong atomic number dependence is not an issue here. So a high dose of radiation can be delivered to superficial skin lesions with limited damage to underlying and adjacent normal tissues. This can be particularly advantageous when the skin cancer to be treated is located over bone or cartilage. In contrast, the high density of bone and cartilage is responsible for a high relative absorption of radiation when X-rays are used, and these tissues are therefore more at risk to develop radionecrosis. For low energy electron beams (2–10 MeV), the dose distribution to the level of 80 % isodose is uniform. As their energies are higher than those of X-rays, electrons can treat thicker lesions much more efficiently [4, 11].
9.3 The Margins
The determination of the margins for lesions treated with electron beams must absolutely take into account the fact that the area of high dose intensity is constricted inside the borders of the radiation fields by as much as 1 cm (blurred field edge). A larger field size than the one used with superficial X-rays may be necessary to cover the target area adequately to counterbalance the penumbra region of the electron beams [4]. To underestimate this physical fact can be responsible for a higher recurrence rate after treatment with electron beams. Tumor localization near the eye is a relative contraindication to perform an electron beam treatment because of the lack of sharpness at the edge of the electron fields. In this case, superficial X-rays are preferable for a better eye protection.
9.4 The Buildup
Because of the electrons’ buildup, the maximum dose is localized under the surface of the skin, and its depth depends on the electron energy. As the target for epithelial carcinomas is the skin, it is essential to use a bolus (tissue-equivalent material) to be placed on the skin. The thickness of the bolus depends on the depth of the buildup [4].
9.5 Local Control and Treatment Modality
Griep et al. have presented a retrospective analysis of 389 basal or squamous cell carcinomas treated either with superficial X-ray (99) or electrons (290). Local or loco-regional recurrence was 4.9 %. The local control of the 99 lesions treated with superficial X-rays was 97 %, whereas it was 94.5 % for the 290 lesions treated with electrons (p = 0.30). Similar rates of local control are reported in the literature [12]. The overall local tumor control rate in the study reported by Locke et al. in 531 patients was 89 % with a median follow-up of 5.8 years [2]. Tapley and Fletcher [2] have reported a local control of 86 % in 156 patients treated for epithelial skin carcinomas with electron beam therapy, with follow-up between 2 and 8.5 years [13]. In Zablow et al.’s analysis, the local control of 115 skin cancers (99 patients) was 88 % with a follow-up between 24 and 47 months [14]. In Miller and Spittle’s study, a primary control of 82 % in 29 patients was found with a follow-up between 2 and 6 years [11].
The results reported above on the local control with electron beam therapy contradict the initial data reported by Lovett et al. in their retrospective analysis on 339 basal (242) and squamous cell (97) carcinomas treated with either superficial X-rays (187), electrons (57), megavoltage photons (15), or combined treatment (80). Overall, local control was achieved in 86 % of the patients: 91 % for basal cell carcinoma and 75 % for squamous cell carcinoma. They found that local control was dependant both on the tumor size and on the modality of treatment. Regarding superficial X-rays, the local control was 98 % for lesions less than 1 cm, 93 % for lesions 1–5 cm, and 100 % for lesions more than 5 cm. Regarding electrons, the tumor control was 88, 72, and 78 %, respectively, whereas for megavoltage photons (60Co, 4 MV photons) tumor control was 100, 67, and 33 % respectively. Finally with mixed treatments, local control was 90, 76, and 64 %, respectively [5]. In an updated analysis after more than 10 additional years, Locke et al. have reported an overall local tumor control rate of 94 % for superficial X-rays modality, of 82 % for electron beam, of 82 % for mixed treatment, and of 50 % for megavoltage photons. Nevertheless, in multivariate analysis, the treatment modality was not significant (electron versus other treatment modalities, p = 0.345). On one hand, these results may reflect an improvement over the years in the use of electrons as a modality of treatment for epithelial skin cancer. On the other hand, electrons were generally used for more advanced tumors than those treated with superficial X-rays, and this can explain the poorer local control in that group [2].
Silva et al. from the Princess Margaret Hospital have reported their experience in the treatment of carcinoma of the pinna. Among the 334 lesions treated, 278 (83 %) were treated with orthovoltage radiotherapy and 39 (12 %) with electron beams. The local control was worse in the group treated with electrons. However, after the correction of the RBE (relative biological effectiveness), there were no more statistically significant increased local failure rates with electrons [15]. The different results reported in the literature for treatment with electron beam therapy are summarized in Table 9.1.
Table 9.1
Studies on skin carcinomas including electron beam therapy
Literature | Number of patients | Follow-up | Local control | Local control in basal cell carcinoma | Local control in squamous cell carcinoma |
|---|---|---|---|---|---|
Locke J 2001 a,b | 531 | 5.8 years | 89 % | 92 % | 80 % |
Superficial X-rays | 317 | 94 % | |||
Electron beam | 100 | 82 % | |||
Combination of treatment | 108 | 82 % | |||
Megavoltage photon | 6 | 50 % | |||
van Hezewijk M 2010 | 434 | 3.6 years (median) | 96.5 % | ||
54 Gy (18 fractions) electron beam | 159 | 5.4 years | 97.5 % (actuarial at 3 years) | 97.6 % (actuarial at 3 years) | 97 % (actuarial at 3 years) |
44 Gy (10 fractions) electron beam | 275 | 2.6 years | 96.1 % (actuarial at 3 years) | 96.9 % (actuarial at 3 years) | 93.6 % (actuarial at 3 years) |
Griep C 1995 | 389 | 1.98 years (average) | 95.1 % | 95.9 % | 92.5 % |









