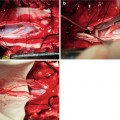
Fig. 11.1
Showing the post-stimulus voiding mechanism
11.3 Dorsal Rhizotomy of the Sacral Nerves
Sauerwein in 1988 structurally expanded SARS with a sacral de-afferentation (SDAF), i.e. dorsal rhizotomy of sacral roots S2 till S5 [3]. A dorsal rhizotomy is important because it suppresses neurogenic detrusor overactivity and detrusor-external sphincter dyssynergia. This results in a low-pressure bladder without reflex contractions of the detrusor and subsequently continence. Moreover, it reduces autonomic dysreflexia [7, 8]. Therefore, a dorsal rhizotomy can also be applied in combination with intermittent catheterization to empty the bladder without implantation of a Brindley stimulator.
11.4 Indications and Contraindications
There are often two types that can characterize the bladder in spinal cord injuries: (1) a flaccid (floppy) bladder, and (2) a hyperactive (reflex) bladder.
The flaccid bladder can be a result of damage to the T12/L1 section and below. For a flaccid bladder, no trigger is detected by the nerves responsible for bladder control and therefore no message reaches the brain. The result is that the bladder can be filled in large volume (good storing function), but cannot be discharged spontaneously. When the urine collected is over the capacity of an adult’s bladder (400 cm3), the urine will back up the ureters and towards the kidneys. The reflux of the urine up the ureters can lead to kidney failure as well as complications, such as urinary tract infection, bladder stone formation, etc. Clinically, one of the more practical forms of management for a flaccid bladder is ICP.
A reflex bladder will be caused when damage to the spine is above the T12 level. For a reflex bladder, the spinal cone still has innervations to the bladder, but lose the upper control from the brain. It is characterized by detrusor hyperreflexia (cause incontinence), detrusor-external sphincter dyssynergia, high bladder pressures and, vesicoureteric reflux leading to renal impairment. The patient can pass urine at anytime and anywhere, which can be rather disconcerting.
Spinal cord injured patients with a suprasacral lesion usually develop a spastic bladder. The neurogenic detrusor overactivity and the overactive external sphincter cause incontinence and threaten these patients with recurrent urinary tract infections (UTI), renal failure and autonomic dysreflexia. All of these severe disturbances may be well managed by sacral deafferentation (SDAF) and implantation of a sacral anterior root stimulator (SARS).
Candidates criteria for patient selection including the following [9]:
1.
Skeletally mature.
2.
Intact reflex bladder contractions, i.e. sufficient efferent nerve pathways to the bladder and the bladder is able to contract. Contractions of at least 50 cm H2O in males, or 30 cm H2O in females need to be present during filling cystometry.
3.
At least 12 months post-injury to ensure stable lesion.
4.
A clinically complete spinal cord lesion.
5.
Preoperative MRI excluding arachnoiditis at the level of the conus and cauda equine.
6.
Good support network.
The contraindications including: (1) Poor or inadequate bladder reflexes, (2) Active or recurrent pressure ulcers, (3) Active sepsis (blood poisoning), (4) having an implanted cardiac pacemaker.
11.5 Surgical Technique
The patient is placed in prone position. The total operation consists two parts: electrodes implantation and dorsal root rhizotomy, and may involve in three or four incisions. Implantation can be performed in introdural or extradural at the sacral root level, deafferentation can be performed at the introdural at the sacral level, or at the conus medullaris at T12-L1 vertabral level (Table 11.1) [10–19].
Table 11.1
Comparison of different surgical procedures
Methods | Skin incision | SARS | SDAF |
|---|---|---|---|
Brindley | L4-S2 | Intradural | Introdural |
Barcelona | L5-S3, T12-L2 | Extradural | Conus |
Tanagho | L4-S2 | Intradural | Posterior ganglion |
L4-S2 | Extradual | Introdural |
1.
Intradural implantation:
A laminectomy from L3-L4 to S1-S2 is done for an intraduralrhizotomy and intradural implantation of the electrode cuff [1]. The dura and arachnoid are opened at midline to expose the sacral nerve roots. The anterior and dorsal components of the roots, especially relevant anterior roots for micturition, can be identified intradurally by electrical stimulation of these components while monitoring the effects on detrusor activity, blood pressure, and somatomotor responses. A rhizotomy of the identified dorsal sacral roots is done. The anterior sacral roots are positioned into the electrode cuff. The connecting cables are subcutaneously tunnelled to a subcutaneous pocket (lateral thoracic) for the receiver.
2.
Extradural implantation:
Implantation of extradural electrodes requires a laminectomy from L5-S1 to S3-S4 [15]. The dorsal rhizotomy is done at the level of the posterior ganglia of S2-S5. Electrical stimulation tests are used to identify the anterior and dorsal components of the sacral roots. The extradural electrode is implanted and fixated to the nerve using a strip of silicone rubber sheet which is sewn to itself and surrounds the nerve. The connecting cables and the receiver are implanted the same way as the intradural procedure.
3.
Surgical Techniques of Barcelona procedure
As a routine, we prefer extradural electrode implantation and SDAF at conusmedullaris (the Barcelona procedure) for our patients, and this will be described in detail [18]. The advantages of SDAF at conusmedullaris is less risk of damaging anterior roots, and almost no risk of failing to completely cut the posterior root. Its disadvantage is two skin incisions and requires more time to removal bone (laminectomy).
The operation usually takes 4–5 h.
If the anterolateral or lateral thoracic site is chosen for the receiver, the whole opertation can be done with the patient prone. If the abdominal or anterior thoracic site is chosen, the patient must be turned to supine for implantation of the receiver block.
Premedication with atropine should be avoided, and if the patient has been taking an antimuscarinic drug, this should have been stopped at least 7 days before the operation. Neuromuscular blocker, if used during operation, should be stopped at the stage of testing the roots by stimulation.
A longitudinal 10 cm skin incision is made from lower lumbar to sacral, centered at S1. Laminectomy from L5 to S3 vertebrae is done, exposing the bilateral nerve roots, including S2, S3 and S4. It is first identified by anatomic locations (L5 nerve root located in L5/S1 vertebrae), and then demonstrated by intraoperative electrical stimulation and observation of the lower leg muscle response (Table 11.2) and bladder pressure uprising (filled with 100 saline water) through indwelling balloon catheter.
Table 11.2
Innervations of sacral root nerve to bladder and lower leg muscles
S2 | S3 | S4 | ||
|---|---|---|---|---|
1. | Detrusor | ± | +++ | ++ |
2. | Sphincters | +++ | ++ | +± |
3. | Sex | +++ | ± | − |
4. | Lower leg muscle | Gluteal major, gultealmedius, femoris biceps, triceps, flexors of hullux and other toes | Triceps, flexors of hullux and other toes | None |
The parasympathetic autonomic efferents from sacral spinal cord to bladder detrusor are generally considered lying in S2-4 ventral roots. In surgery, it is very important to determine the innervative frequency and efficacy of every individual nerve root when operation is performed on the sacral roots. We performed those operations in ten cases of Chinese with complete supraconal spinal cord injuries. There were seven men and three women, with an average of 32 years old. Our results show that pressure contributions are provided by S3 roots in all ten patients, bilaterally; and by S4 roots on the right side of ten patients and left side of eight patients. However, only three have minimal pressure uprising by S2 stimulation, one on the right side and two on both sides. The mean innervative efficacy by differential sacral roots to bladder detrusor is shown in Fig. 11.1. S3 root is the most frequent and the most efficacious contributor, S4 is the second frequent and a lesser but still significant efficacious one, and S2 is the last frequent and the minimal contributor(Fig. 11.2) [20]. The right roots seem to be stronger than the left ones. The efficacy distribution of sacral root innervation to bladder detrusor obtained by us is similar to that by Brindley, but the innervative frequency is different. Rising in bladder pressure is obtainable always by stimulating S3, usually by S4, and often by S2 in Europeans; however, it is always by S3, usually by S4, and seldom by S2 in Asians [20].
Fig. 11.2
Differential sacral roots innervation to bladder detrusor in Asian people
The tripolar electrode (arranged with middle cathode and upper and lower anodes) is attached to a strip of silicone rubber (6 mm wide and 39 mm long). One end of this silicone rubber is passed under the appropriate segmental nerve (S2) or nerves (S3 and S4 together). Then the two ends of the rubber strips are sutured. Be careful to check the tension when suturing. The strip of the silicone rubber should be just loose enough to allow a little sliding, avoid nerve entrapment. The upper and lower anodes should be laid within a few millimeters to the nerve. It is not important whether they touch it.
When all the electrodes are in place, the cables are tunneled through to the receiver site, and the block of receivers are implanted.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree