Fig. 1.1
Heel pressure ulcer: a spreading infection is observed some days after the necrotic tissue appeared

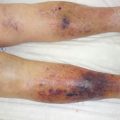
Fig. 1.2
A tigh haematoma presenting an “iceberg like” situation. The necrotic skin hides a large undermined zone of dissecting blood, source of potential infection
Fig. 1.3
(a, b) Progressive necrosis of the distal phalanx in a renal insufficient patient submitted to an arterial thief after arteriovenous fistula for hemodyalisis
Diabetic foot ulcers may become necrotic at toe level, with a distal complete dry necrosis, and mummification can be expected (spontaneous evolution towards spontaneous amputation). In most cases skin necrosis is reduced to a small black spot with a large cavity hiding behind, the foot becoming oedematous and inflammatory. Pus will leak from different zones on the foot, usually the dorsum and the interdigital spaces, proof of large infected soft tissues, osteoarthritis affecting joints of the foot. Large early debridement may prevent amputation if carried out rapidly, in close collaboration with the vascular surgery team in order to prevent renecrosis.
1.5 How to Manage Skin Necrosis
1.
Wet to dry is a technique used in the past to eliminate debris on the wound
Classically, the technique involves applying a wet gauze soaked in sterile water and waiting for its desiccation. When dry, it will be removed together with crusts, pus and debris. This technique is painful and will harm the granulation tissue, inducing local haemorrhage.
2.




Progressive autolytic debridement
Conservative solutions such as dressings providing moisture (autolytic debridement) will induce a progressive release and detachment of undesired tissues over the wound. Hydrogels are the most used dressing at home, the nurse moisturising the wound one day and gently removing the sloughy tissue the next. This less painful technique allows better psychological management, curettage of a leg ulcer every 2 days inducing a poor quality of life. Mechanical debridement remains extremely painful and should be reevaluated in the light of the new dressing performances, the capacity to remove metalloproteases from the wound surface, and using local antiseptics or irrigating fluid. Negative pressure wound therapy was proposed as a possible treatment for soft necrotic tissue [3], a promising strategy still under evaluation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree