CHAPTER 9 Disorders of the Sesamoids
EVALUATION
Making the correct pathologic and clinical diagnosis of sesamoid disorders can be difficult, although distinguishing between an acute and a chronic pathologic process involving the sesamoids, as required to identify a bipartite sesamoid, for example, is fairly straightforward. In the case illustrated in Figure 9-1, the patient was a 27-year-old runner who presented with acute pain around the hallux metatarsophalangeal (MP) joint, and it was difficult to determine whether the pain was in the joint or reflected a sesamoid problem. The plain radiograph demonstrated a bipartite morphology for both the tibial and the fibular sesamoids.
A bipartite sesamoid may be painful, the result of acute injury, with diastasis between the fragments. Figure 9-2 is the forefoot radiograph of a 29-year-old marathon runner who presented for treatment of acute pain under the sesamoids. Note that the tibial sesamoid is bipartitite and is slightly larger than the normal-sized fibular sesamoid. The fibular sesamoid, which was painful, demonstrates a diastasis of the distal pole (the sum of the two parts of the fibular sesamoid is normal, whereas the sum of the two parts of the tibial sesamoid is greater than it should be). This finding helps in diagnosis, and in the case illustrated, the acutely fractured fibular sesamoid was excised.
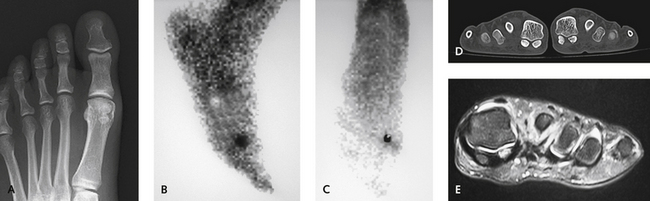
When the diagnosis is in doubt, additional imaging studies such as computed tomography (CT), magnetic resonance imaging (MRI), and technetium bone scan may be helpful, as in the case depicted in Figure 9-3. The patient was a professional tennis player with diffuse pain under the first metatarsal, and on the plain radiograph, neither sesamoid was normal: the tibial sesamoid was bipartite, and the fibular sesamoid appeared to be avascular. Bone scan, CT scan, and MRI confirmed avascular necrosis of the fibular sesamoid, which was excised.
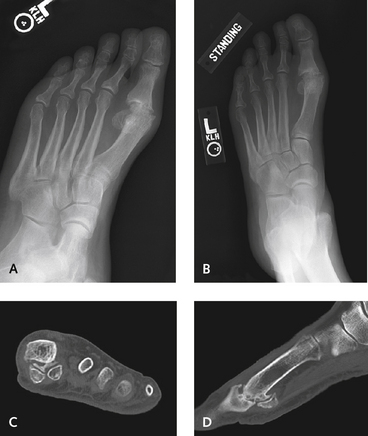
Further imaging studies may be helpful in other circumstances as well. In Figure 9-4, the patient was a 44-year-old woman who presented with significant pain associated with hallux rigidus. The alternative of an arthrodesis and interposition arthroplasty was discussed with her, but the radiographic appearance was worrisome because of the arthritic changes in the sesamoid-metatarsal complex. If arthritis is present, arthroplasty may not be the correct procedure, because pain under the hallux MP joint may persist postoperatively. A CT scan confirmed presence of arthritis (see Figure 9-4), so an arthrodesis of the MP joint was recommended.
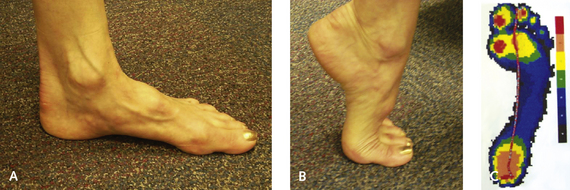
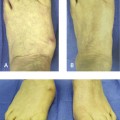
In evaluating the sesamoids and the hallux MP joint, assessment of the dynamic range of motion is important: At what point does the joint become painful? Where exactly is the pain located? Is the pain reproduced with pressure? In Figure 9-5, the patient was a 31-year-old recreational runner with a cavus foot who presented with the complaint of pain under the tibial sesamoid. The passive range of motion of the MP joint was excellent, with good dorsiflexion, but pain was present at the midrange of motion of the hallux. Significant equinus of the first metatarsal, with increased pressure under the first metatarsal head, was demonstrated on the pedobarogram (see Figure 9-5, C). If a sesamoidectomy is performed in a patient with a cavus foot, the pressure will shift to the adjacent fibular sesamoid or the undersurface of the metatarsal head. Thus a tibial sesamoidectomy is not a good option for this patient, regardless of the underlying pathologic process. After orthotic management failed to provide pain relief, a dorsiflexion osteotomy of the first metatarsal was recommended.
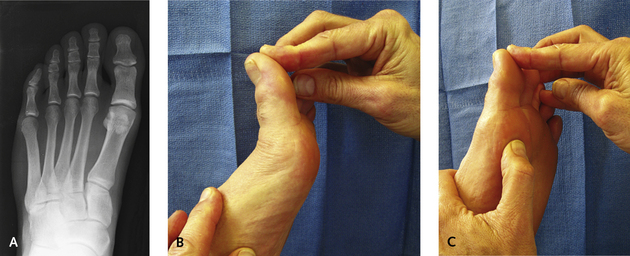
Dynamic range of motion of the MP joint is important to assess after injury, with determination of the location of pain in particular and of the position of the sesamoids with passive dorsiflexion. Figure 9-6 illustrates the case of a patient with chronic pain under the first metatarsal head, with bipartite tibial and fibular sesamoids. Pain was present during passive dorsiflexion of the hallux and simultaneous application of pressure on the sesamoids. With this more diffuse pain, a sesamoidectomy is contraindicated, because removal of one sesamoid will only increase the pain under the remaining sesamoid. The focus of management must therefore be on use of orthotic support; if this fails to provide clinical improvement, then an osteotomy of the first metatarsal can be performed if its position at rest is in plantar flexion or equinus. If the metatarsal is in neutral position and therefore is not the source of the increased pressure, it may be necessary to remove the more symptomatic of the two sesamoids. Bone grafting of the abnormal bipartite sesamoid also could be considered.
After injury, the static and dynamic positioning of the sesamoids must be determined with radiographs taken during weight bearing. Retraction of one or both sesamoids or half of the fractured or bipartate sesamoid must be recognized if present. In Figure 9-7, the patient was a professional football player who presented with acute pain after a hyperextension injury to the left hallux. Subtle proximal retraction of both sesamoids with such injuries is suggestive of a rupture of the plantar plate (see Figure 9-7, A). This was confirmed on passive dorsiflexion lateral radiographs of both feet (see Figure 9-7, B and C). Note the position of the sesamoids in the right foot (see Figure 9-7, B) relative to their more proximal location in the left foot (see Figure 9-7, C). The sesamoids in the left foot clearly are not moving with the sesamoid complex in passive dorsiflexion of the hallux, thereby confirming rupture of the volar plate complex. In the case shown in Figure 9-8, a similar diagnosis was made of an acute volar plate injury, also in an American football player. The plain radiograph (see Figure 9-8, A) demonstrates the fracture of the tibial sesamoid and the slightly proximal position of the fibular sesamoid. This is a more difficult diagnosis, because chronic problems may already have been present in the fibular sesamoid, as was confirmed on MRI scan (see Figure 9-8, B) in this patient.