(1)
Department of Dermatology, Drexel University, Philadelphia, Pennsylvania, USA
Abstract
Meyerson’s nevus and Doucas Kapetanakis pigmented purpuric dermatosis are two completely disparate diseases that both have eczema as a feature. Meyerson’s nevus is an ordinary nevus with eczema surrounding it. Doucas Kapetanakis involves a pigmented purpura along with eczema on the lower legs. Clinically, these two diseases are easily recognizable, but pathologically they are challenging. On hematoxylin and eosin stain we have found occluded sweat ducts in the epidermis adjacent to Meyerson’s nevus. These blockages were periodic acid–Schiff positive. The fact that the findings in both these diseases are similar to ordinary eczema helps substantiate the hypothesis that eczema is associated with occluded sweat ducts and that the occlusions arise from biofilms.
Keywords
BiofilmsCapillaritisDoucas KapetanakisEczemaHalo nevusMeyerson’s nevusOccluded sweat ductsPigmented purpuric dermatosisSchamberg’s diseaseSpongiosisTwo diseases, completely disparate, have eczema as a feature. One is Meyerson’s nevus, which is an ordinary nevus with eczema surrounding it (Fig. 1.21). The other is the Doucas Kapetanakis type of pigmented purpuric dermatosis (PPD), which involves pigmented purpura along with eczema (Fig. 8.1). Clinically, these entities are easily recognizable; however, pathologically they are a bit more challenging.


Fig. 8.1
Doucas Kapetanakis pigmented purpuric dermatosis. On the lower leg are pigmented purpuric macules and two pink papulovesicular plaques
Meyerson’s Nevus
Meyerson’s nevus clinically is a pigmented papule with a surrounding pruritic, pink to red, papulovesicular plaque. Scaling or crusting may be secondary features of the surrounding plaque. The scaling and crusting may also extend to the nevus [1]. The description is thus that of a “halo” nevus, but instead of the ordinary white halo, an eczematous plaque surrounds the pigmented nevus [2]. The sequelae of the two “halo” type lesions are different also. With topical corticoid treatment, the plaque around the Meyerson’s nevus resolves, leaving the central mole. The outcome in the halo nevus is destruction of the nevus with the entire area becoming white. This resulting white patch repigments over time. As an aside, many important lessons could be learned from this process because, in the halo nevus, the melanocytes get destroyed by the lymphocytic infiltrate, leaving a vitiliginous patch that, over time, repigments (think melanoma and vitiligo).
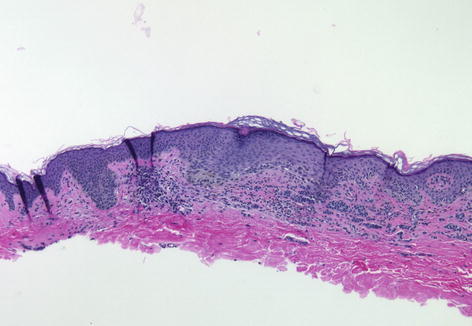
The pathology of Meyerson’s nevus shows an intradermal or compound melanocytic nevus with the plaques and strands of ordinary nevus cells with ordinary maturation and architecture. In other words, it is a completely normal nevus. A patchy lymphocytic infiltrate is present in the dermis along with prominent epidermal spongiosis and focal lymphocytic exocytosis [1]. The lymphocytes are all normally sized and shaped (Fig. 8.2). In the halo nevus, the lymphocytes specifically infiltrate into the nevus cell nests and create a dense, band-like, high-hugging, lichenoid infiltrate in the upper dermis. No spongiosis is present in the halo nevus. Thus, the spongiosis and the nature of the lymphocytic infiltrate have been the differentiating points in the pathology of these two diseases, since they were first described.