(1)
Yotsuya Medical Cube, Chiyoda-ku, Tokyo, Japan
Basic Principles
Avulsion and degloving injuries of the finger and hand where the skin is stripped off large areas are accompanied by exposure of bone and tendons, and how fast repair of the skin can be carried out is the key to recovering function post-surgery. For the reconstruction method, it is best to combine different methods based on the level of the injury.
It is important to reconstruct the skin defect area by combining various methods, and to commence hand therapy as soon as possible after surgery to prevent contracture of the finger joints.
Selectable Flaps and Surgical Procedures
Abdominal subcutaneous pocket insertionAbdominal flapFree temporal fascial flapReverse flow radial forearm flapExtended twisted wrap-around flapThe difficulty level of each surgical procedure is shown subsequent to the procedure title (e.g., Level of Difficulty: 2). The levels range from 1 to 5, with level 1 indicating a preliminary level and level 5 indicating a very advanced level.
4.1 Temporary Coverage: Abdominal Subcutaneous Pocket Insertion (Level of Difficulty: 1)
Information
First, comprehensive debridement is carried out to the crush wound, and necrotic and infected tissue resected. A subcutaneous pocket is created in the abdomen, the crushed finger or hand inserted inside and the surrounding area sutured closed. The purpose of this surgery is not to cover the wound using the skin of the abdominal wall, but only to conduct temporary tissue banking.
This can be done under local anesthetic.
4.1.1 Operation Procedures

Fig. 4.1
Procedure 1: Re-attachment was conducted for a degloving injury, however progression of necrosis continued

Fig. 4.2
Procedure 2: Debridement is conducted under local anesthetic and necrotic soft tissue completely resected

Fig. 4.3
Procedure 3: The entire thumb is inserted into the abdominal subcutaneous pocket

Fig. 4.4
Procedure 4: Appearance after removing one week later. The progression of necrosis of the bone and tendon tissue has been stopped. A twisted wrap-around flap was then used to cover the skin defect area
Tips
Prior to reconstructing a hand or finger, another option is to temporarily cover the area using a pedicled abdominal flap
If there is insufficient soft tissue on the graft bed, a large sacrifice is made by the foot when a toe transplant is conducted. For cases with large skin defects, it is a practical measure to conduct a vascularized abdominal flap as a preliminary treatment to conducting a toe transplant.


4.2 Free Temporal Fascial Flap (Level of Difficulty: 4)
Information

Fig. 4.5
Procedure 1: Degloving injury of hand accompanying wide-area crushing injury
Vascular pedicle Superficial temporal blood vessels
Advantage Extremelythin. Useful for covering exposed tendons and bones of hands and feet. Donor scar isn’t obvious on haired area. Possible to harvest two temporal fascial flaps
Disadvantage Hemorrhagic. Requires careful attention to stop bleeding. If dissection layer is too superficial can lead to hair loss. Harvesting of deep fascia is somewhat complex. Too thin to be suited to reconstruction of the palmar finger tip.
Indication When an area needs to be covered using thin tissue (mainly reconstruction of dorsum of hand)
(Hirase, Y., et al.: Reconstruction of degloving injuries. Plastic Surgery Advance Series. Plastic surgery for the limbs. Recent Progress, Editing: Kojima, T., pp 134–142, Kokuseido Publishing, Tokyo, 2005)


4.2.1 Operation Procedures

Fig. 4.6
Procedure 2: An incision is made in the temporal area in line with the path of the superficial temporal artery, and after broadly dissecting the upper fascia, the required fascia is flap is severed. The temporal fascia flap peels off easily by using fingers, so following the superficial temporal artery in the proximal direction, the temporal fascia flap is completely elevated and harvested
Refer to Section of
“Reconstruction of Dorsum of Hand/Free temporal fascia flap” in Chap. 3




Fig. 4.7
Procedure 3: The exposed bone and tendon are covered with the temporal fascial flap, and anastomosis is performed with the superficial temporal blood vessels to the radial blood vessels in the snuff box

Fig. 4.8
Procedure 4: A split-thickness skin graft is conducted on top of the fascia flap

Fig. 4.9
Procedure 5: Appearance 3 weeks after surgery. (Part of photos reproduced from Hirase, Y: Reconstruction using free flaps. Plastic Surgery for Injuries. pp 127–132, Kokuseido, Tokyo, 2007)
4.3 Reverse Flow Radial Forearm Flap (Level of Difficulty: 3)
Information
Vascular pedicle Reverse blood flow of the radial blood vessels and the anastomotic cutaneous vein
Size Excluding the skin directly above the ulnar artery, possible to use almost all of the skin on the forearm
Advantage Skin is flexible and thin. There are few restrictions on the design, and it is possible to harvest flaps in a range of shapes. The vascular pedicle is large, and because it is possible to perceive the palpitations through the skin, flap design can be conducted accurately. Can also be used as an adipofascial flap without inclusion of the skin.
It is also possible to include tendon or part of the bone in the flap.
Disadvantage A skin graft scar will be seen on the exposed section. Circulation from the radial artery will be sacrificed
4.3.1 Operation Procedures

Fig. 4.10
Procedure 1: The design is created with the pivot point of the blood flow for the flap placed distal of the snuff box
Refer to Section of
“Reconstruction of the dorsum of the hand/Reverse flow radial forearm flap” in Chap. 3
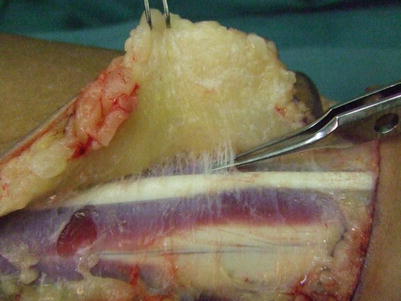
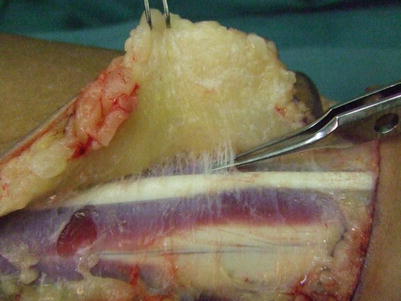
Fig. 4.11
Procedure 2: Elevation begins from the ulnar margin of the flap. With the antebrachial fascia attached to the flap, detachment and elevation is conducted above the proper fascia
Note
Because the antebrachial fascia is not actually involved in the blood flow for the flap, the flap can be elevated with it on the tendon side, however the technique is complex.


Fig. 4.12
Procedure 3: Confirmation is made of the radial artery entering the flap at the intermuscular septum where the antebrachial fascia becomes thicker
Note
In the area surrounding the intermuscular septum, fascia of around 2–3 cm in width must be included in the flap.
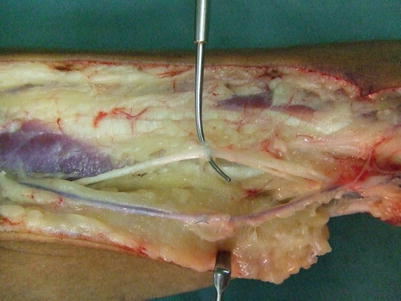




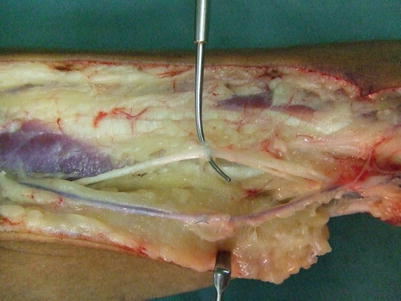
Fig. 4.13
Procedure 4: An incision is made in the radial margin, and the flap is detached from above the proper fascia with the antebrachial fascia included in the flap. The cutaneous vein is included in the flap, with care taken that the dorsal branch of the radial nerve and the thick radial cutaneous vein is retained without being damaged

Fig. 4.14
Procedure 5: With the radial blood vessels included, the intermuscular septum is detached from the periosteum. During the procedure conducted up until now, it is possible to confirm several cutaneous branches from the radial artery

Fig. 4.15
Procedure 6: When the full length of the radial blood vessels are detached, the flap is separated from the forearm, and attached only to the vascular pedicle. The cutaneous vein in the flap is secured so that it can be used for anastomosis later on

Fig. 4.16
Procedure 7: Case: Skin defect present on volar side of right thumb and degloving injury to index and middle finger

Fig. 4.17
Procedure 8: Under a local anesthesia, the index and middle fingers are placed in an abdominal subcutaneous pocket, and the skin defect of the thumb is covered with a local skin flap
Note
The MP joints are temporarily fixed with a steel wire so that they don’t flex.