Anterior Cruciate Ligament Healing and Advances in Imaging
Keywords
• Anterior cruciate ligament • Healing • Imaging • Magnetic resonance imaging • Plain radiography • Computed tomography • Vascularization • Maturation
Key Points
Introduction
Advances in imaging have provided clinicians with powerful, noninvasive methods to assess the progress of a patient in the healing process. Magnetic resonance imaging (MRI) has been used to assess the healing process of articular cartilage, menisci, and ligamentous structures.1–3 The utility of these tools in anterior cruciate ligament (ACL) reconstruction continues to evolve as clinicians attempt to understand the impact of graft healing on patient outcomes. Perhaps most importantly in ACL reconstruction is the ability for a graft to tolerate the required forces for a patient to return to sport. There is tremendous variability in the literature regarding return to sport following ACL reconstruction, with reports ranging from 33% to 92%.4,5 This variability suggests patients may be returning to sport before the reconstructed ACL is able to tolerate the forces necessary to do so. Ideally a patient would return to sport once the reconstructed ACL had matured. As a result, methods to assess graft maturity and healing are important clinical tools in assessing which stage each individual has reached in the progression of graft healing and maturation. These tools may also be helpful in developing physical therapy protocols and deciding when an athlete is allowed to return to sport.
Graft maturation
The “ligamentization” process, by which an ACL graft undergoes healing and remodeling, has been studied histologically in animal models and, to a lesser degree, in humans. Numerous animal studies have shown a process involving revascularization, cell repopulation, and metaplasia of the tendon tissue to a ligamentous appearance.6,7 Although the ligamentization process in animals has correlated well with human studies, the time frame in which this process occurs has been shown to take longer in humans.
The stages of graft healing and maturation have been divided into early, remodeling, and maturation, although there does not seem to be a consensus on the timing of these stages.8–12 Studies have shown increasing vascularity in the early phase, establishing the groundwork for graft remodeling and healing. This increase in vascularity will slowly decrease as remodeling progresses toward a tissue that histologically resembles the native ACL. Although visualization under light microscopy provides direct information regarding revascularization, studies on ACL graft healing in humans are difficult to perform, given their invasive nature and the need to remove tissue from the reconstructed ACL. MRI provides a noninvasive means to evaluate revascularization, as represented by an increased signal intensity of the graft and periligamentous tissue.
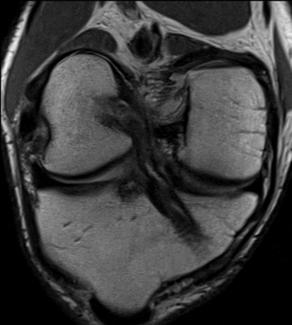
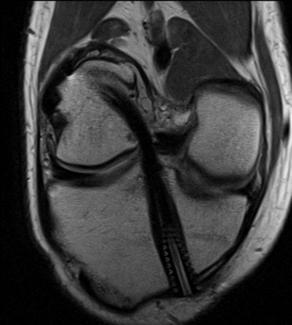
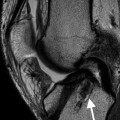
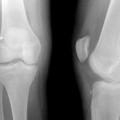
Studies have shown that MRI may be used to determine graft vascularity by correlating to signal intensity. Several studies have described methods to assess graft vascularity using MRI. On proton density (PD)-weighted sequences, an increase in signal appears to correlate with increased vascularity (Fig. 1). Graft signal will then decrease as the graft matures (Fig. 2). Ntoulia and colleagues13 studied this finding in human subjects undergoing autograft bone-patellar tendon-bone ACL reconstruction. Contrast-enhanced MRI was used to evaluate graft vascularity by calculating the Enhancement Index (ratio between the signal-to-noise quotient [SNQ] after contrast and before contrast). Thirty-two male patients were evaluated at postoperative day 3, as well as 6 and 12 months after surgery. No increase in graft signal intensity was seen 3 days after surgery. The intra-articular graft site showed significant enhancement at 6 months, with no significant increase at 12 months.
Gohil and colleagues14 used MRI to evaluate the effects a remnant-sparing minimal debridement technique may have on revascularization in subjects undergoing autologous hamstring ACL reconstruction. The investigators reported earlier revascularization in the minimal debridement group at 2 months in comparison with standard reconstruction techniques. Although histologic studies have confirmed the presence of a vascularized graft as early as 3 weeks, the findings of these studies correlate with the increase in vascularity described in histologic studies.11
MRI has also been useful in comparing healing between autograft and allograft tissue. Marumatsu and colleagues15 compared remodeling between autogeneic and allogeneic bone-patellar tendon-bone grafts in patients undergoing ACL reconstruction. Contrast-enhanced MRI was performed at 1, 4, 6, and 12 months after surgery, with occasional MRIs obtained up to 72 months after. An SNQ was calculated as described by Weiler and colleagues.16
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree