CHAPTER 10 Correction of Lesser Toe Deformity
CLAW TOE AND HAMMERTOE CORRECTION
I follow a simple algorithm for correction of claw toe and hammertoe:
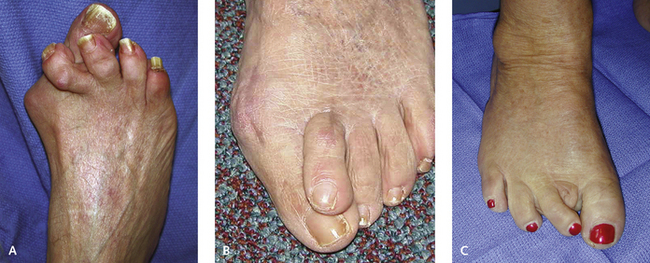
In establishing the optimal approach to a claw toe or hammertoe deformity, it is important to distinguish a vertical plane deformity from a horizontal plane deformity such as the crossover toe deformity. The latter can never be corrected with an interphalangeal joint arthroplasty, because the apex of the deformity is not the IP but the MP joint (Figure 10-1). Certain deformities are very difficult to correct as a result of intrinsic contracture. These include, for example, the deformities associated with the complications of crush injuries of the forefoot or secondary to a compartment syndrome. The muscle fibrosis and intrinsic contractures shorten the flexor brevis muscle, and tenotomy is never sufficient. Correction of the fixed IP joint deformity will straighten the toe but will not improve flexibility at the MP joint, and the stiffness frequently is more debilitating. If indeed the toe is straightened, and the MP joint is stiff, toe pain will be worse, because the pressure on the tip of the toe increases. Typically, the toe can be extended slightly with the MP joint in flexion, but if the toe is extended, then the fixed, contracted nature of this deformity becomes more apparent (Figure 10-2). In addition to correction of the fixed contracture at the PIP joint, the MP joint requires release by shortening the metatarsal and relative lengthening of the intrinsic muscles. Even this procedure is not always sufficient, and metatarsal head resection may be necessary, particularly after crush injuries of the forefoot. What is the best approach to toe deformities in the elderly associated with asymptomatic hallux valgus? Clearly, the incidence of recurrent deformity of the toes will be high if the hallux is not simultaneously corrected. It frequently is the second or third toe, however, that is markedly dislocated or fixed at the PIP joint. Can an isolated toe procedure be performed with any expectation of a predictable result? If the hallux is overriding the second toe, it is possible to perform the toe surgery without correcting the hallux deformity, as illustrated in Figure 10-3. In this case, the patient had bilateral painful second and third toe deformities, but the hallux was fairly rigid after a previous resection arthroplasty. After the corrective surgery, the toes are straight and the hallux lies dorsal to the toes.
Another option for surgical management of the painful second toe is amputation (Figure 10-4). This is an excellent treatment in the presence of an isolated painful toe deformity or a fixed asymptomatic hallux valgus, or cases in which the hallux cannot realistically move into any further valgus because it is already abutting the third or fourth toes (see Figure 10-4, B). Toe amputation also may work well in the patient who has undergone an arthrodesis of the hallux MP joint (see Figure 10-4, C). This approach is a good alternative, particularly with a grade IV crossover second toe dislocation. When the amputation of the second toe is performed, it is very important to eliminate all sources of pain, including the plantar surface of the metatarsal head. A logical assumption might be that with amputation, there is no pressure on the metatarsal, so metatarsalgia will be relieved. This is not the case, however, and I have encountered a patient who experienced persistent pain under the metatarsal head after amputation. The likely cause is subluxation of the fat pad from under the metatarsal head, so that even after amputation, pain under the head can persist. In such patients, I always remove the plantar condyles at the same time as the amputation.
CORRECTION OF THE METATARSOPHALANGEAL JOINT CONTRACTURE
I approach the MP joint release sequentially. The procedure begins with a release of the long and short extensor tendons, followed by a transverse dorsal capsulotomy. If a contracture still persists, I release the collateral ligaments dorsally and then, finally, release the volar plate contracture, if present. If the joint is unstable or dislocated, soft tissue releases as described for a contracture are not sufficient, and a shortening osteotomy of the metatarsal needs to be performed. If the MP release is performed as an isolated procedure, in the absence of correction of the IP joint, then a decision has to be made whether to secure the MP joint with a Kirschner wire (K-wire), which should be used judiciously. There is always the potential for breakage of the wire, and in particular, infection with consequent chronic swelling may be a problem (Figure 10-5). These infections take a very long time to settle down, and the toe may remain swollen for months. If I detect any unusual swelling or inflammation in the toe after placement of a K-wire, it is removed promptly, and a debridement of the joint performed if necessary. The K-wire should never be used to reduce an unstable joint, because the subluxation will recur promptly once the wire is removed. In other words, the K-wire can facilitate scarring of the MP joint, but it should not be relied on to correct deformity.
PROXIMAL INTERPHALANGEAL RESECTION ARTHROPLASTY AND ARTHRODESIS
Either a longitudinal or a transverse elliptical incision is made over the posterior interphalangeal (PIP) joint, over a length of approximately 1 cm. I use small hooks to retract the skin and then incise the extensor hood either longitudinally or transversely. Choice of the incision depends on whether arthroplasty or arthrodesis is performed and whether K-wire fixation of the joint is used. In elderly patients, I prefer to use strapping instead of a K-wire to stabilize the toe, and in these patients, I use a transverse ellipse over the PIP joint and can close the ellipse to help with the alignment of the toe. This transverse incision does, however, cause some thickening of the PIP joint, which is permanent. Once the distal portion of the PIP joint is identified, the collateral ligaments on either side are cut. The cut is directed inward toward the joint, to prevent accidental laceration of the neurovascular bundle. A curved periosteal elevator (named a shmogler by Dr. Melvin Jahss) is inserted into the IP joint to strip the soft tissue from the medial lateral surface and undersurface of the phalangeal neck (Figure 10-6).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree