Chapter 17 Correcting Deviated Noses, Septoplasty and Turbinectomy
Online Contents
In this Chapter Online at experconsult.com
Correcting Septal Tilt Animation 17.2
Osteotomy to Reposition a Deviated Nasal Spine Animation 17.3
Correcting Septal Tilt to the Right Internally and to the Left Externally Animation 17.4
Placing Spreader Grafts Controls Anterior Curvature Animation 17.6
Illustration Showing Correction of a C-shaped Cephalocaudal Deviation Animation 17.8
Illustration Demonstrating Correction of an S-shaped Anteroposterior Deviation Animation 17.10
Illustration Showing Correction of an S-shaped Cephalocaudal Deviation Animation 17.12
Placing a Septal Rotation Suture Animation 17.14
Correcting Caudal Deviation of the Nose Animation 17.15
Reducing the Projection of the Lower Lateral Cartilage on One Side Animation 17.16
Repositioning a Deviated Nasal Base Animation 17.17
Correcting Tip Deviation and Adjusting the Lower Lateral Projection Animation 17.18
Pearls
• Commonly, the deviated nose and septum are associated with other conditions such as sinus headaches, frequent sinus infections and migraine headaches.
• Nasal deviation and valvular dysfunction following facial paralysis offers the best evidence regarding the role of the soft tissues in nasal symmetry and valve function.
• A longstanding shift of the midline structures cannot be simply corrected with an osteotomy and forceful repositioning. It requires component separation and realignment of all of the structures individually, including the nasal bones, the septum and the upper lateral cartilages.
• Mid-vault deviation consistently accompanies anterior, and commonly, mid and posterior septal deviation.
• Of the six classes of septal deviation, the most common is the septal tilt in which the septum itself has no significant underlying curvature but it is tilted to one side because the caudal septum is dislodged to one side of the vomer bone (often the left side).
• The C-shaped anteroposterior deviation is the second most common type of septal deviation.
• A persistent unilateral obstruction of the airway is a reliable indicator of a mechanical airway compromise.
• A negative history of airway obstruction is not a reliable indication of a patent airway since the patients may not have a basis for comparison.
• Many female patients with nasal deviation pluck their eyebrows differentially to camouflage the nasal asymmetry, which can be misleading. On these patients, the mid-eyebrow point should not be used as the upper face midline.
• In patients who have frequent sinus headaches, sinus infections, or migraine headaches, a CT scan may disclose pathology such as septal deviation, sinusitis, concha bullosa, septa bullosa, contact points and Haller’s cell.
• A medial deviation of the nasal bone requires an outfracture of the bone that will be supported with an extended spreader graft to avoid medial shift of the bone while it is healing.
• A longstanding deviation of the anterior nose will require separation of the upper lateral cartilages from the midline and repositioning.
• A cardinal step in correction of most deviations, especially tilt, is disengagement of the dislodged caudal portion of the retained alar strut from the vomerine groove and anterior nasal spine, removal of the redundant, overlapping cartilage and repositioning and fixation to the nasal spine periosteum, as long as one is confident that the anterior nasal spine is positioned in the midline.
• If the anterior nasal spine is deviated, it has to be osteotomized and repositioned.
• Components of correction of anteroposterior C-shaped deviation include removal of the posterocephalic portion of the septum and the deviated portion of the perpendicular plate and vomer bone, repositioning of the posterocaudal septum, and rarely, scoring of the septum and placement of splints on either side of the septum.
• Correction of C-shaped cephalocaudal deviation requires removal of the posterocephalic portion of the septum, release of caudal tension and repositioning the L-frame, scoring the concave side if release of tension would not correct the deviation.
• Whenever the septum is scored, application of extramucosal stents is necessary to control and maintain the septum straight while it is healing.
• For correction of S-shaped deviation, the posterocephalic portion of the septum is removed and the caudal portion of the L-frame is repositioned, the concave side is scored, if necessary, and extramural splits and spreader grafts are applied.
• If an inadvertent tear in the mucoperichondrium is unilateral, it will not be consequential. If the tear is bilateral but the perforations are not apposing, the mucosa may still heal without persistent perforation. When the tears are apposing, a straight piece of septal cartilage or perpendicular plate is replaced and the extramural stents are applied for two to three weeks.
• The remaining caudal dorsal deviation can be corrected using a septal rotation suture. This is a horizontal mattress suture placed through the upper lateral cartilages and the septum more cephalad on the side that the structures will be rotated towards.
• A deviated caudal nose is often associated with disparity in the length of the lower lateral cartilage. Depending on the tip projection, one has to either elongate the short lower lateral cartilage or shorten the long side to rotate the tip to the midline.
• The notion that the turbinates may shrink after correction of the deviated septum is ill-conceived and illogical. Rather than shrinking, the enlarged turbinates may shift the septum off the midline.
Pathology
The soft tissue envelope with its underlying perinasal musculature plays a major role in maintaining the symmetry and patency of the valvular mechanism. Nasal deviation and valvular dysfunction following facial paralysis offers the best evidence regarding the role of the soft tissues in nasal symmetry and valve function. The perinasal musculature was discussed in Chapter 1.
The septum constitutes the main central support for the nose, which is composed of the perpendicular plate, the quadrangular cartilage and the vomer bone (see Figure 1.17 in Chapter 1). The perpendicular plate of the ethmoid is in continuity with the posterior edge of the quadrangular cartilage and both structures are aligned caudally with the vomer. The most anterocaudal portion of the septal cartilage also rests on the maxillary crest in a tongue-and-groove relationship. This point of articulation is unique in that the perichondrium of the cartilage is only partially contiguous with the periosteum of the crest, allowing a decussation of fibers that joins the contralateral perichondrium.1 This configuration can make a submucoperichondrial dissection tedious. Starting the dissection from the posterior caudal septum and continuing it in the anterior direction may overcome the difficulty. This relationship between the cartilage and the bone renders this portion of the septum susceptible to post-traumatic displacement of the cartilage from the groove of the crest, correction of which is paramount for the successful straightening of the septum and consequently the external nose.
Adjustment of the size of the turbinates plays a cardinal role in the restoration of nasal function following correction of nasal deviation. The inferior turbinate occupies a large portion of the nasal airway and can account for up to two-thirds of the total airway resistance.2 The turbinates are covered with an erectile mucosal tissue composed of pseudostratified ciliated columnar epithelium. The submucosa contains many seromucinous glands and vascular channels containing cavernous sinusoids. These channels are under the influence of the autonomic nervous system and thus serve as the end target for decongestant medication. The sympathetic system regulates the resistance vessels (and therefore blood flow) and the parasympathetic system regulates the capacitance vessels (and therefore blood volume) of the nasal mucosa. The submucosa also contains large numbers of mast cells, eosinophils, plasma cells, lymphocytes, and macrophages. Thus, chronic inflammation secondary to stimulation of these abundant proinflammatory cellular constituents can lead to fibrous deposition and chronic hypertrophy of the turbinate.1 Long standing deviation of the septum, especially if it occurs at an early age, results in enlargement of the inferior and/or middle turbinate facing the concave side of the septum (Figure 17.1).
The internal nasal valve accounts for approximately 50% of the total airway resistance and is the narrowest segment of the nasal airway.3,4 It is formed by the angle between the junction of the nasal septum and the caudal margin of the upper lateral cartilage and is typically 10–15°, as mentioned in earlier chapters5 (see Figure 1.13 in Chapter 1).
The importance of the nasal valves in nasal airflow cannot be overstated and has been studied extensively.6–9 The internal nasal valve is a crucial regulator of nasal airflow dynamics and should be preserved and/or reconstructed during rhinoplasty. Injury and destabilization of this complex, by either surgery or trauma, may result in collapse and subsequent nasal airway obstruction. The external nasal valve, which serves as the entrance to the nose, is formed by the caudal edge of the lateral crus of the lower lateral cartilage, the soft tissue alae, the membranous septum, and the sill of the nostril (see Figure 1.13 in Chapter 1). This is an occasional site of obstruction secondary to extrinsic factors, such as foreign bodies, or intrinsic factors, such as weak or collapsed lower lateral cartilages, a loss of vestibular skin, or cicatricial narrowing.5 Normal function of this valve depends on the structural integrity of the lower lateral cartilages, the perinasal musculature, and adequate soft tissue coverage. Functional compromise can occur with encroachment of the nasal spine, and especially the footplates, into the nostril opening. Architecturally weak lateral crura further compound the effects of a widened columella.10 Other causes for external valve collapse include facial nerve palsy, pinched alar deformity, and postsurgical vestibular stenosis secondary to synechiae and over-resection of the lower lateral cartilages.
The septum and the nasal bones control the direction of the nose. Thus, deviation of the nose can result from misalignment of one or the other, or a combination of both. Often, the nasal bones follow the direction of the deviated septum. However, these structures may move independently. Midvault deviation consistently accompanies at least anterior and commonly mid- and posterior septal deviation. Deviation of the lower nose may involve the caudal septum, anterior nasal spine, and lower lateral cartilages. Previous studies by the author’s team and others have detailed and categorized the types of septal deviation.5,11–14
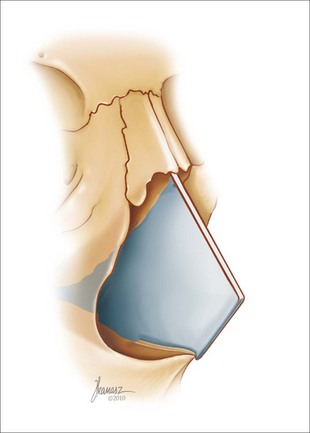
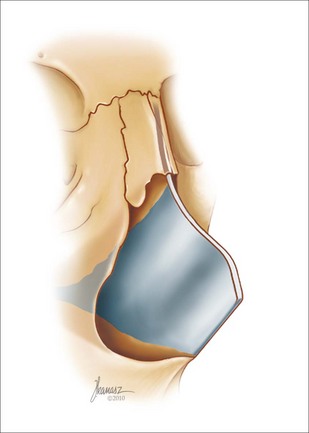
There are six classes of septal deviation.11 The most common type is a septal tilt, in which the septum itself has no significant underlying curvature but is tilted to one side because the caudal septum is dislodged to one side of the vomer bone (Figure 17.2). In most cases of septal tilt, the internal dislodgement of the septum is to the left and the external deviation of the nose is to the right. This is usually accompanied by an enlargement of the inferior turbinate ipsilateral to the external deviation.
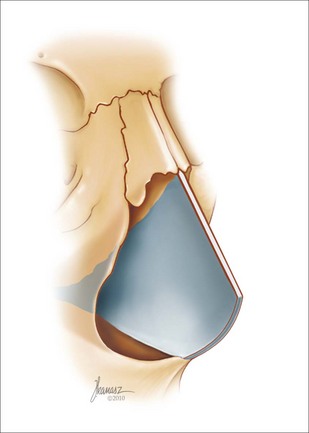
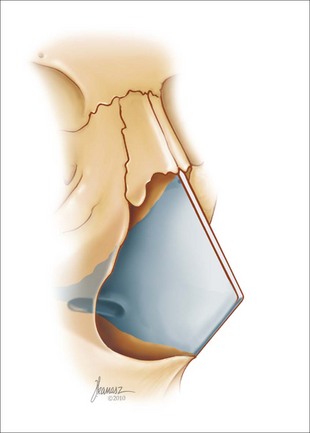
C-shaped anteroposterior deviation is usually associated with deviation of the vomer plate. External reflection of the anteroposterior C deviation is often similar to the septal tilt (Figure 17.3). In addition to the enlargement of the inferior turbinate, the middle turbinate is often enlarged as well.
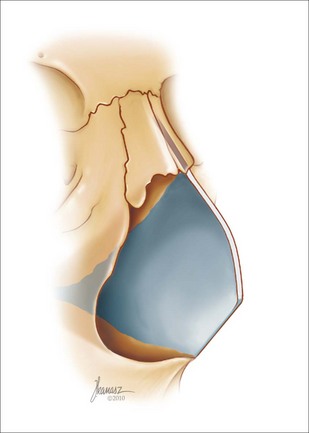
C-shaped cephalocaudal deviation presents externally as a curved appearance of the nasal dorsum. The most common form of this deviation is the reverse C with the curve facing the patient’s right (Figure 17.4). The opposing inferior, and often the middle, turbinate is enlarged.
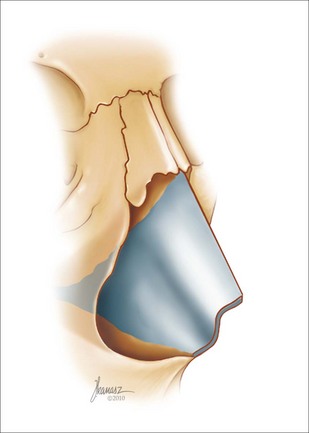
S-shaped anteroposterior deviation is defined by two opposite curvatures in continuity in the anteroposterior direction (Figure 17.5). Externally, the anteroposterior deviation will present with a shift of the nose to the left or right. Rarely, the anterior portion of the nose may look totally straight.
S-shaped cephalocaudal deviation is similar to the previous type except that the curvatures are in the cephalocaudal direction (Figure 17.6). Inferior and middle turbinate enlargement is common with both types of S-shaped deviations. The external nose follows the pattern of the septal deviation.
The last type of septal deviation is a localized deviation or spur. This is a purely functional problem and has no translation to the external shape of the nose (Figure 17.7).10 Turbinate enlargement is not common with this type of deviation.
Patient Assessment
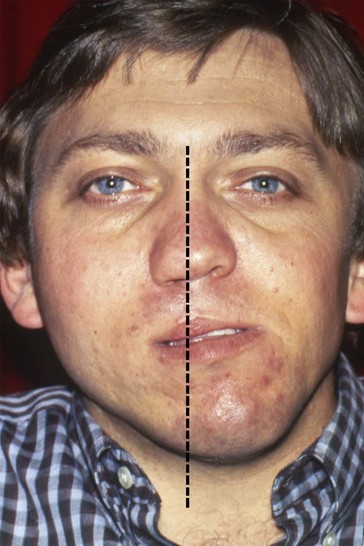
Attention to detail and careful observation are vital in order to garner the critical information necessary to arrive at the correct diagnosis and an effective surgical plan. Observation of the external nose and face should include attention to oral or nasal breathing. Mouth-breathing can be continuous or intermittent. Additionally, the face should be assessed for overall symmetry, canting of the plane of occlusion, and alignment of the nose with the rest of the facial structures (Figure 17.8). The chin position should be noted in relation to the upper face midline, the upper and lower lips. and the midline of the upper and the lower incisors. The midline should be set at the intercanthal line rather than the intereyebrow plane. Many female patients with nasal deviation pluck their eyebrows differentially to camouflage the nasal asymmetry, which can be misleading (Figure 17.9). On these patients, the mid-eyebrow point should not be used as the upper face midline. Examination of the oral cavity may reveal a very high and narrow palatal arch that encroaches on the nasal airway. Such patients commonly have a very constricted nasal airway and require special care to maintain and perhaps widen it (Figure 17.10).
Facial nerve function is also assessed, since paralysis of the perinasal muscles can cause nasal airway obstruction. The nose is then observed zone by zone for deviated structures, including the nasal bones, the anterior septum, the upper and lower cartilages, and the lower lateral cartilages, similarly to the procedure described in Chapter 2
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree