By its very nature, a revision surgery is made up of difficult choices. A cosmetic procedure that requires revision is even more so. In the case of revision rhinoplasty, the surgeon is faced with a task that has both aesthetic and functional ramifications. It is the complexity of this surgical endeavor that has engendered such a wide range of opinion. Not surprisingly, the controversy surrounding revision rhinoplasty begins at the very start of the process with patient selection. Multiple surgical approaches are available, and their merits are debated. Methodology for the correction of functional compromise is equally diverse, with a variety of proponents for individual corrective procedures. In revision rhinoplasty, the surgeon is often left with a paucity of the preferred autogenous grafting materials, and the controversy surrounding the use of synthetic implants is discussed. In brief, the controversy concerning revision rhinoplasty surgery stems from the intensely personal nature of the procedure. The wide range of opinions on how best to approach the revision patient is a testimony to the fact that no one perfect approach exists.
 Patient Selection and Timing of Surgery
Patient Selection and Timing of Surgery
When a patient who has undergone a primary rhinoplasty is dissatisfied with the results, a choice must be made. The patient must decide if he or she would like the original surgeon or a new one to assume the responsibility for the revision surgery. All surgeons who do rhinoplasties will at some point be faced with one of their own patients who desire revision. In addition, the busy rhinoplasty surgeon will be asked to consult with the patients of other surgeons. When dealing with a patient from your own practice or another surgeon’s patient, the initial counseling stage is vital. Patients will ask about the timing, the cost, and the nature of their revision procedure.
The relatively standard period of time to wait from a primary to a revision procedure has been 12 months. Ostensibly, this has been determined to be the optimal time to return to the nose in terms of postoperative scarring and edema. In addition, this waiting period allows the patient to realize fully the outcome from his or her original procedure. A significant cosmetic change that was difficult for the patient to feel comfortable with may be perfectly acceptable after the interval 12 months. Conversely, subtle inequities in tip contour or dorsal form may not be appreciated until this time period has elapsed. For the majority of our own patients, we continue to advise that they allow this full time period to pass before deciding on revision. Counseling for this waiting period can be more difficult if the patient has come to the office from another practice. This patient group is often unhappy with their primary surgeon and wants a rapid resolution to the perceived problem. It is not uncommon to have the initial consultation with this patient group within a few months of primary surgery.
A handful of unique situations exist in which we will pursue a revision procedure before the 12-month waiting period. One group of patients in whom early revision is advised is the functional patient. A patient who has undergone a functional restoration may present in the early postoperative period with incomplete resolution. Further examination may reveal a previously unaddressed aspect of their dysfunction. An example would be the patient undergoing an internal nasal valve procedure who postoperatively presents with previously unrecognized external valve collapse. We do not hesitate to revise these patients. Another group of patients who may undergo early revision is those with extruded alloplastic implants. These patients can benefit from immediate revision to avoid a time interval in which they have to live with the deconstructed nose. In addition, removal of the alloplastic implant may result in contracture of the soft-tissue envelope, and immediate replacement can help prevent this. A study by the senior author has shown that immediate reconstruction with irradiated rib homograft is a safe, viable option for this procedure. 1
One of the attendant problems of revision rhinoplasty is the cost involved with the procedure. Many patients who present for potential revision underwent their primary surgery on a cash-pay or flat-fee basis. When revision is required the question often arises: who will pay for the surgery? If a patient has come to our practice from another physician, the conversation regarding financial matters is kept very simple. For patients with postrhinoplasty dysfunctional nasal breathing, we offer to obtain preapproval from the patient’s insurance carrier. Should that fail, the case will proceed on a flat-fee basis. At no time do we become involved in the process of collecting a fee from the prior physician. Those finances are strictly viewed as a matter between patients and their primary rhinoplasty surgeon. Furthermore, we will not actively participate in any ongoing legal action that involves a patient seeking our surgical care. When one of our patients requires revision, the formulation of the procedure cost is also kept very simple. For patients whose original procedure was paid for by insurance, we will once again attempt preapproval for their case. For flat-fee patients who require revision, we do not charge an additional surgical fee; we do, however, ask the patient to cover the costs of anesthesia and operating room fees.
Male patients undergoing secondary rhinoplasty require special consideration. In general, male patients are less proficient and open at expressing what aesthetic results they desire from the procedure.2 As a result, the preoperative consultation becomes especially important to firmly establish the surgical goals. In addition, the acceptable aesthetic range of the male nose is somewhat narrower than that found in female patients.3 Men presenting for secondary rhinoplasty may present with a feminized appearance and may require careful counseling before they accept augmentation rhinoplasty as a revision procedure. Finally, male patients with heavy sebaceous skin who desire additional refinement may be advised not to pursue further surgery.
There has been significant debate regarding rhinoplasty in adolescence as a primary procedure. Secondary rhinoplasty is therefore even more controversial. The majority of adolescent patients seeking rhinoplasty are female.4 Recent psychosocial investigations have demonstrated that these young women are very capable of making accurate decisions regarding cosmetic surgery. The self-perception and insight into the decision for surgery was demonstrated to approximate that of their parents.5 Although their decision to seek primary rhinoplasty may have been formed on sound principles, the surgeon must be very careful when approaching revision surgery in adolescents. The major concern in our practice is the anticipation of cutaneous changes that patients undergo as they move from adolescence into early adulthood—namely, how thicker more sebaceous skin may transform to the thinner skin of adulthood (Fig. 16–1). The prudent primary rhinoplasty surgeon will anticipate this and counsel the patient against overly dramatic contour changes. However, even with the best preoperative counseling, some adolescent patients will be unhappy with their conservative result. When these patients present for possible secondary surgery, the revision surgeon has the responsibility of not only analyzing the patient’s current aesthetics but also envisioning the nasal appearance for years to come. Only then can the correct decision regarding further surgery be made.
Finally, there is the subset of rhinoplasty patients who have had multiple previous surgeries and continue to desire alteration of their nasal appearance. These patients may suffer from body dysmorphic disorder (BDD). BDD is defined as a preoccupation with an imagined defect in one’s appearance or excessive concern over a real but minor cosmetic flaw. Approximately 5% of all patients seeking cosmetic rhinoplasty may suffer from this psychiatric condition.6 We will not operate on patients we believe suffer from BDD. The exception to this rule is the patient with BDD who has significant function impairment from previous cosmetic rhinoplasty. For these cases, we recommend that the patient seek and complete professional counseling before further surgery is discussed.
 Types of Anesthesia
Types of Anesthesia
The approach to secondary rhinoplasty starts with the selection of anesthetic type. Part of the decision will be predicated on the patients’ experiences with their prior procedure. In our practice, many patients have strong opinions regarding their prior anesthetic experience—both positive and negative. Our preference is always to perform the procedure under local anesthesia with sedation. We will vary from this approach, depending on the anesthetist available, patient profile, and extent of surgery. Because we practice in the university setting, we do not always have an anesthesiologist comfortable with intravenous sedation anesthesia. When this occurs, rather than struggle, we will convert to general anesthesia. Similarly, if a patient has a high level of anxiety regarding the procedure, we always make general anesthesia available. For patients undergoing major reconstructive rhinoplasty, we prefer general anesthesia because of the anticipated duration of the procedure. Much of the literature regarding anesthesia choice for nasal surgery comes from the management of blunt nasal trauma. This literature supports the safety of either choice.7 A large recent study of cosmetic rhinoplasty patients verified that the procedure could be performed successfully with intravenous sedation or intravenous sedation with dissociative anesthesia.8 In the end, the choice of anesthetic is made between the surgeon and patient after careful consideration of all the options.
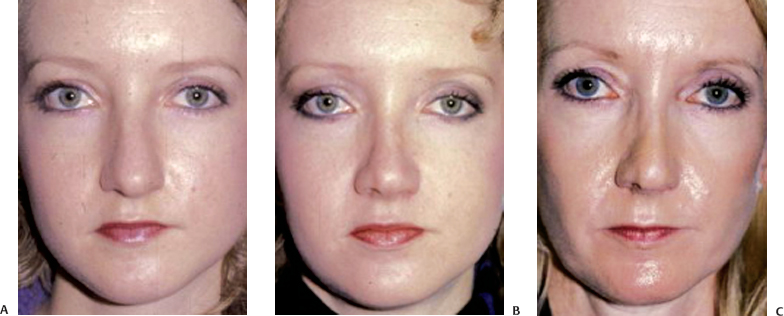
Figure 16–1 Demonstration of the skin changes that occur during the transition from the teen to adult years. A noticeable decrease in skin thickness and overall refinement is observed. Patient has undergone reduction rhinoplasty.
 Level of Intervention
Level of Intervention
The general approach to revision rhinoplasty can be classified as minimalist or maximalist. The minimalist approach is best defined as performing the simplest procedure or procedures to restore the aesthetic and functional deficits. A maximalist approach similarly seeks to restore the functional and cosmetic defects but does so in as a complete a fashion as possible. Wong and Giammanco illustrated the minimalist approach in a study from 2003.9 They described the preservation of septal cartilage in isopropyl alcohol. Patients who presented postoperatively with contour irregularities underwent revision surgery with the placement of crushed cartilage grafts through isolated incisions. By contrast, the maximalist approach was illustrated by Romo et al.10
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


