Chapter 9 Contact dermatitis
1. Name the two pathogenic types of contact dermatitis.
Contact dermatitis refers to cutaneous inflammation resulting from the interaction of an external agent and the skin. These reactions occur through one of two mechanisms: a nonimmunologic irritant contact dermatitis (ICD) or an immunologic allergic contact dermatitis (ACD). ICD accounts for 80% of all reactions, while ACD is responsible for approximately 20%. Although over 3700 substances have been identified as contact allergens, almost any substance, under the right circumstances, can act as an irritant. It is important to note that irritating compounds can be allergenic, and allergenic compounds can be irritating.
Marks JG, Elsner P, DeLeo VA: Contact and occupational dermatology, ed 3, St Louis, 2002, Mosby.
2. Name the two subtypes of irritant contact dermatitis, and describe them.
ICD can be divided into acute toxic and cumulative insult subtypes. Acute toxic eruptions occur from a single exposure to a strong toxic chemical, such as an acid or alkali, inducing erythema, vesicles, bullae, or skin sloughing. Reactions occur within minutes to hours after exposure, localize to the areas of maximal contact, and have sharp borders. In most cases, healing occurs soon after exposure. Chronic cumulative insult reactions are the more common type of ICD. These are due to multiple exposures of many low-level irritants, such as soaps and shampoos, over time. This dermatitis may take weeks, months, or even years to appear. It is characterized by erythema, scaling, fissuring, pruritus, lichenification, and poor demarcation from the surrounding skin.
3. Explain the pathogenesis of allergic contact dermatitis (ACD).
ACD is a type IV, delayed, cell-mediated, hypersensitivity reaction. Initially, a low-molecular-weight antigen hapten (<500 Daltons) contacts the skin and forms a hapten–carrier protein complex. This complex then associates itself with an epidermal Langerhans’ cell, which presents the complete antigen to a T-helper cell, causing the release of various mediators. Subsequently, T-cell expansion occurs in regional lymph nodes, producing specific memory and T-effector lymphocytes, which circulate in the general bloodstream. This whole process of sensitization occurs in approximately 5 to 21 days. Upon reexposure to the specific antigen, there is proliferation of activated T cells, mediator release, and migration of cytotoxic T cells, resulting in cutaneous eczematous inflammation at the site of contact. This phase occurs within 48 to 72 hours after exposure. Because many allergens are irritants, preceding irritation is common and may enhance allergen absorption. In contrast to irritant reactions, relatively small concentrations of an allergen can be enough to elicit an inflammatory reaction. Acute ACD may have erythema, edema, and vesicle formation. Chronic ACD reactions are scaly, erythematous, possibly lichenified, and can mimic chronic ICD. Table 9-1 compares ACD and ICD.
Table 9-1. Comparison of Irritant and Allergic Contact Dermatitis
| IRRITANT | ALLERGIC | |
|---|---|---|
| Examples | Water, soap | Nickel, fragrance, hair dye |
| Number of compounds | Many | Fewer |
| Distribution of reaction | Localized | May spread beyond area of maximal contact and become generalized |
| Concentration of agent needed to elicit reaction | High | Can be minute |
| Time course | Immediate to late | Sensitization in 2 weeks; elicitation takes 24–72 hrs |
| Immunology | Nonspecific | Specific type IV delayed hypersensitivity reaction |
| Diagnostic test | None | Patch test |
Li L, Cruz P: Allergic contact dermatitis: pathophysiology applied to future therapy, Dermatol Thera 17:219–223, 2004.
4. Can urticarial reactions occur from contact with a substance?
Occasionally, urticarial reactions may occur with certain exposures, instead of the eczematous changes seen with ACD and ICD (Fig. 9-1). Allergic contact urticaria involves a specific IgE–mast cell interaction, resulting in the release of vasoactive compounds. While urticaria occurs at the site of contact, more generalized symptoms can appear, including angioedema, anaphylaxis, rhinoconjunctivitis, and widespread urticaria. A good example is the latex glove immediate reaction reported in health care professionals. Nonimmunologic contact urticaria occurs secondary to a non–antibody-mediated release of vasoactive mediators or due to a direct effect on the cutaneous vasculature. Many agents found in cosmetic products can cause a nonimmunologic contact urticaria. These include sorbic acid, benzoic acid, and cinnamic acid. This may explain the facial burning and stinging that some patients experience using cosmetics. To diagnose contact urticaria, a prick test is usually performed. In this test, a small amount of the allergen is placed on the skin, and a needle is used to prick the skin. An urticarial wheal of appropriate size constitutes a positive test, usually developing within 15 to 20 minutes after allergen administration (Fig. 9-2).
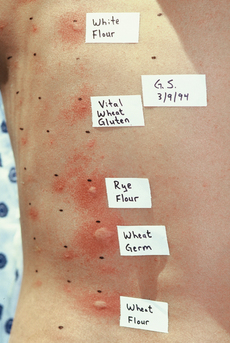
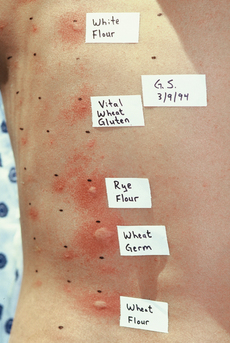
Figure 9-2. Prick test for the diagnosis of contact urticaria. The patient was a baker allergic to flours and wheat.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree









