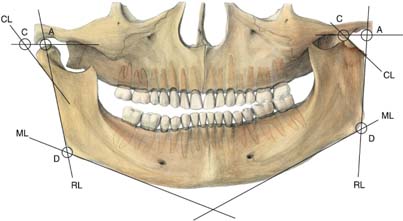
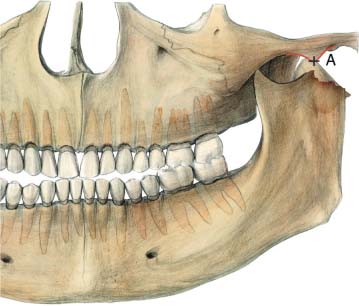
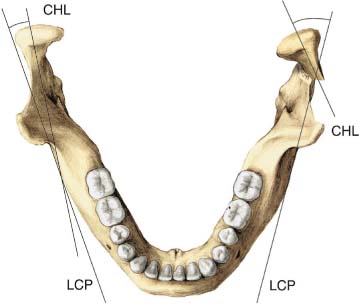
13 Condylar Neck Fracture Miniplates: Extraoral Approach Early mobilization and functional rehabilitation are considered important in the treatment of condylar neck fractures (Zide and Kent, 1983; Upton, 1991). Although indications for various treatment methods remain controversial, open reduction and internal fixation are generally required for fractures with severe displacement or dislocation (Zide, 2001). Anatomically correct repositioning and functional stabilization of such a severely displaced fracture require sufficient exposure of the fracture site, with good access and visibility through an extraoral approach. The miniplate is one of the most commonly used devices for fracture fixation. Simple radiographic measurements (panoramic, radiograph, and Towne’s view) are used to identify difficult condylar fractures. Silvennoinen et al. (1994) found that fractures with marked reduction in ramus height, irrespective of presence or absence of condylar displacement, frequently resulted in occlusal and functional disturbances (Figs. 13.1–13.3). Condylar displacement from the fossa is not the only deciding factor. Where the condyle is still in the fossa, reduction of more than 8mm in ramus height is frequently associated with a therapy-resistant occlusal change. In cases in which the condyle is dislocated from the glenoid fossa, overriding is also evident. Because of condylar displacement, marked reduction of ramus height is also observed (mean 10.3 mm). Thus we consider traumatic reduction of more than 8 mm in ramus height to be an indication for surgery. In an extensive epidemiological study on different patterns of condylar fractures, Silvennoinen et al. (1992) pointed out that 15 % of patients were retrospectively considered to have had an indication for open reduction. Fig. 13.1 The method of radiological measurement. Ramal height is the distance between the mandibular line (ML) and a tangent to the superior point of the condyle (CA) measured along the ramus line (RL) on the fractured and nonfractured sides (from point A to point D). Reduction of ramus height is represented by the difference in length between the fractured and nonfractured sides. The mandibular line is the tangent to the lower border of the mandible. Fig. 13.2 Dislocation. The fracture is considered to be dislocated when the condyle is located in front of the lowest point of the articular eminence, or when the angulation in an oblique frontal projection (Townes view) is more than 50°. Fig. 13.3 Measurement of fracture angle. Angulation of the fractured and nonfractured condylar processes is measured in the oblique frontal projection as the difference between a midcondylar line (CHL) and a line along the lateral cortical plate (LCP) of the mandibular ramus. Angulation of the fractured side is represented by the difference, in degrees, between the fractured and nonfractured sides. Two main approaches are preferred: the preauricular approach and the retromandibular approach, with the rhytidectomy (face-lift) approach as a modification (Fig. 13.4). The level of the fracture and the degree of displacement are the most important factors in selecting the approach. Preauricular incision is the most direct approach to high subcondylar and neck fractures. It is especially useful for fracture displacements where medial exploration is desired, with the potential for surgical manipulation of soft tissues within the joint (Chuong and Piper, 1988). On the other hand, access to the ramus fragment is often too limited to allow enough space for a miniplate. A retromandibular approach provides good access in cases of low subcondylar fractures, and more space for placing the plate and screws. Subcondylar fractures and fractures extending into the upper ramus region are best addressed using the retromandibular approach. However, reduction of the medially dislocated condyle is often difficult due to the limited access. In severe anteromedial fracture dislocations an additional vertical ramus osteotomy, followed by removal of the osteotomized segment, may be necessary (Boyne, 1989; Ellis, Reynolds and Park, 1989;Mikkonen et al., 1989). Occasionally a combination of approaches is needed, particularly in fracture dislocations in which a preauricular approach may be necessary to retrieve the condylar segment, while fixation is performed through a retromandibular approach (Takenoshita, Ishibashi, and Oka, 1990). The preauricular approach (Al-Kayat and Bramley, 1979) is recommended. The skin incision is carried through the skin and superficial fascia to the level of the temporal fascia. This layer is dissected downward, along and posterior to the temporal vessels, until the lower end of the skin incision is reached. Then the posterior end of the zygomatic arch can be palpated easily. At a point roughly 2cm above the zygomatic arch, the temporal fascia splits into the lateral and medial layers. The pocket formed by the division of the temporal fascia contains fatty tissue, which is visible through the thin lateral layer (Fig. 13.5
Introduction
Indication
Surgical Approaches
Surgical Technique
The Preauricular Approach
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree