Serum total protein
6.0–8.0 g/dL
Serum albumin
3.5–5.0 g/dL
Prealbumin
19–43 mg/dL
Hemoglobin
Female: 11.5–12.5 g/dL
Male: 14.0–18.0 g/dL
Hematocrit
Female: 33–44 %
Male: 39–40 %
Serum transferrin
200–400 mg/dL
Total lymphocyte count
1,500–4,000/mm [3]
These values may vary according to the standard lab value. In addition, we have observed that serum cholesterol drops tremendously in patients with malnutrition. Serum prealbumin determines the status of patient nutrition at the time of testing; with a short half-life, 2–3 days, it is a very sensitive test. Patients with pressure ulcer have been observed to have a low-level value on this test [18]. The author considers the value of the test to be an important factor in determining the nutritional status of the patient and the action required accordingly.
In patients with pressure ulcers, serum albumin is at low levels. For proper healing after surgery ideally, the level should be 3.5 g/dL or above as a preoperative value. Patients with a level of serum albumin above 3.5 g/dL have a lower incidence of pressure ulcer development [10]. Low serum albumin can produce edema under the skin, and skin becomes less elastic and interferes with transfer of oxygen and nutrients from blood to the skin [19]. The edematous area may have a temporary loss of blood flow secondary to increased tissue pressure [17]. A diet rich in calories and protein is recommended to improve serum albumin level. Our clinical observation is that, after closing of the pressure ulcer in a patient with adequate postoperative nutrition, it takes at least 4–6 weeks for serum albumin to achieve a normal level.
Hemoglobin and Hematocrit
Low levels of hemoglobin and hematocrit reduce oxygen supply to the tissue, thus impairing the healing of pressure ulcers. Anemia is found in nearly all the patients with deep or multiple ulcers [20]. This may be caused by the low nutritional status of the patient, including low levels of protein and albumin. Iron therapy is not recommended to correct lower levels of hemoglobin or low hematocrit because the anemia could have resulted from the inability to use stored iron and not from iron deficiency [21]. In severe anemia secondary to sepsis, blood transfusion may be necessary before surgery. The author recommends that patients should have a hemoglobin level of at least 10 g/dL before surgery.
Total Lymphocyte Count
A total lymphocyte count less than 1,500 mm [3] is a risk factor predisposing in development of pressure ulcer. The cause of this low level could be non-nutritional and associated with overwhelming infection and the use of steroids that compromise the immune system of the body.
6.2.4 Calories (Energy) and Protein
Calories are required to fuel all essential body processes and it is important, when giving a high-protein diet, to take into consideration that each gram of nitrogen needs about 150–200 kcal to be utilized by the body. Patients with pressure ulcers need more energy than other patients, especially if they have a spinal cord injury. The explanation for the increased energy expenditure is the underlying chronic inflammatory process involving cytokines and cortisol [18]. It is estimated that patients with pressure ulcers need about 30–40 kcal/kg of body weight/day [22]. Protein is essential for tissue growth and the recommended total protein requirement for patients with stage IV pressure ulcers is 1.5 g–2.0 g/kg of body weight [22].
6.2.5 Micronutrients
Deficiencies in micronutrients, zinc, vitamin C, vitamin A, and vitamin E are associated with poor wound healing. However, there is no strong evidence indicating that deficiency in these supplements is a risk factor in pressure ulcer development. Zinc is known to be involved in the structure of protein, particularly collagen. It is recommended to give oral zinc sulfate in doses of 220 mg/day in the acute stage of wound healing. Vitamin C plays an important role in the hydroxylation of praline and lysine during collagen formation. Optimal wound healing may occur with vitamin C intake of 10–20 mg daily, the same as when 500 mg of vitamin C is given daily [23]. Vitamin A deficiency results in delay of wound healing, but it is not highly recommended to give it routinely because of unproven benefits and potential toxicity.
Vitamin E
There is no strong evidence that vitamin E improves healing of pressure ulcers. Vitamin E may work synergistically with antioxidants like vitamin C to promote wound healing. In summary, vitamins and minerals should be given when clinical deficiency is suspected in patients with severe pressure ulcers and post-surgery.
6.2.6 Methods of Delivering Dietary Intake to Patients with Pressure Ulcers or Post-surgery
Nutritious high-calorie, high-protein daily meals will likely be recommended by the dietician. When a patient is reported as not eating well, a calorie count should be ordered for three successive days to determine the exact number of calories/protein intake per day. Based on the results, plan should be put in action to overcome dietary insufficiencies.
Oral Supplements
There are many commercial supplements available on the market that can be obtained without a prescription. The usual intake is a can of supplement with each meal. This supplement provides 1.0–2.0 cal/mL. If the patient does not like the supplement, a milkshake or protein bar can be substituted. Patients with diabetes or renal failure require a special supplement designed for these diseases. It has been observed that providing these supplements with daily meals helps to heal pressure ulcers to a greater extent than the unsupplemented group of patients [16].
The Use of Anabolic Steroid
In patients in a catabolic state secondary to open wound and sepsis, a consequent loss of appetite and weight is commonly seen in clinical practice. An anabolic steroid is used in these circumstances to increase appetite and weight gain. An examples of a steroid used in clinical practice is oxandrolone; the starting dose is 2.5 mg by mouth three times/day, which can be increased up to a total of 20 mg/day. Another drug is a derivative of progesterone called Megace® (megestral acetate), which is given in a dose of 625 mg or 5 mL/day. Side effects of these anabolic hormones are numerous, the most important being effects on the liver, requiring monitoring of liver enzymes for elevation.
Tube Feeding (Nasogastric Tube)
When a patient who is required to have a high calorie/protein intake has a functional gastrointestinal tract but cannot tolerate a high volume of dietary intake by mouth, a tube feeding is indicted. There are many tube feeding formulas that can be used without side effects like diarrhea, which is a result of quick shift of fluid from the gut secondary to hyperosmolarity of the formula used. Tube feeding can be tolerated for 4–6 weeks. Aspiration pneumonia is a serious complication, therefore, patients with tube feeding should be placed in a semi-sitting position. Our clinical experience shows that young patients refuse tube feeding. Tube feeding can be given at night and in the daytime, and the patient can take regular meals without feeling full. In patients with the need for long-term feeding due to inability to swallow, for example, in high tetraplegia and advanced neurological disease, a PEG tube is recommended. The same precaution to avoid aspiration pneumonia as in tube feeding should be considered; however, sitting too high in the bed, at 90°, increases pressure over the sacral or ischial area even if the patient is on a specialty bed. This can cause a breakdown of the skin in the anatomical areas or a breakdown in the surgical flap.
Total Parenteral Nutrition (TPN)
When tube feeding cannot be used secondary to mechanical obstruction of the gastrointestinal (GI) tract (e.g., because of prolonged ileus, severe GI bleeding, severe diarrhea or vomiting), TPN should be used to deliver nutrition at this stage. TPN requires a central line placement and carries the risk of serious complications, including sepsis and thrombophlebitis of the vein. Elevated glucose levels in the blood can be controlled by giving insulin. Frequent lab tests are required to monitor for elevated liver enzyme, disorders of mineral and electrolyte balance, and acid base abnormality. The author’s clinical indication for using TPN is when patient has a serious catabolic condition, with severely low level of albumin and prealbumin, and needs extensive reconstructive surgery, taking into consideration that the surgery itself can cause a severe catabolic state. For this reason, TPN is used for 2–3 weeks before and after surgery, especially if the patient is required to have a diverting colostomy prior to flap surgery. The use of TPN should be followed by close monitoring of all metabolic conditions of the patient.
6.3 Control of Muscle Spasms and Joint Contractures
The medical history obtained for patients with spinal injury or neurological disease presenting with pressure ulcer should include history of spasticity and type of medication prescribed and its effectiveness. Muscle spasms are common in high-level spinal cord injury (upper motor neuron lesion). Spasms increase in intensity and duration when the patient suffers from stresses like infection or pain. Spinal cord injured patients consider spasms in the lower extremities as a form of movement to help aid the patient in transfers. The side effect of muscle spasms in these patients is that they can predispose in developing pressure ulcers when the patient cannot sit in a wheelchair or when laying in bed in an improper position. In these cases, patients have greater pressure on the skin in some areas than others, which can produce skin breakdown. Muscle spasms can act as shearing forces, for example, over the heel or medial surfaces of the knee area, where pressure ulcers can develop. Severe spasticity can cause subluxation of the hip joints and rotation of the greater trochanter posteriorly; a pressure ulcer can develop over the area, as the greater trochanter will become a pressure point in the sitting position instead of the ischial tuberosity. The effects of muscle spasms during the operation for flap surgery can make it difficult to position the patient on the operating table (Figs. 6.1a, b).
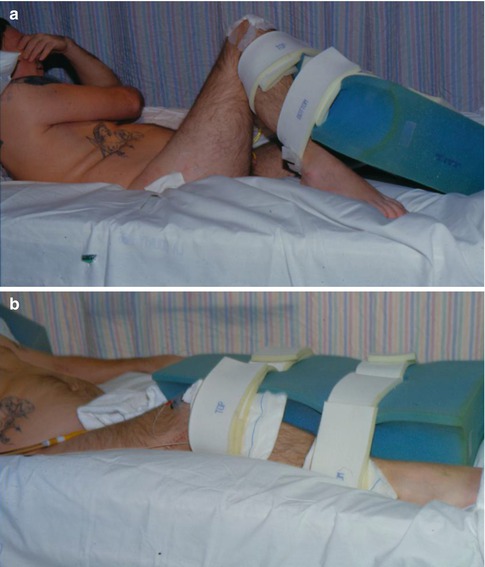
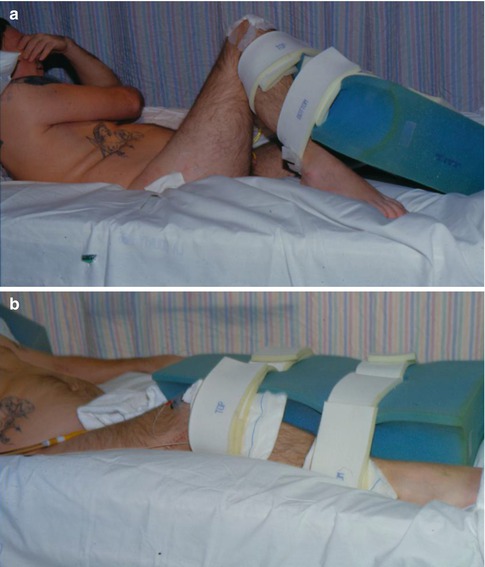
Fig. 6.1
(a) Spinal cord injury patient with severe spasticity at the hip and knee joint, even with the use of abduction pillow. (b) The same patient post nerve injection by phenol to control muscle spasms. Bilateral limbs are in relaxed position
The effect of general anesthesia may sometimes help to control spasticity and allow placement of the patient in the prone position. In the postoperative period, uncontrolled muscle spasms risk flap wound dehiscence [24]. The author’s clinical observation is that the flap wound may develop serious discharge, preventing the sealing of the wound and predisposing to infection. Spasms can also prevent healing of the flap as a result of development of a seroma under the flap. This can be observed by an increase in the amount of drainage in the surgical drainage system, which indicates that some shearing is occurring between the flap and its bed secondary to spasm forces.
6.4 Medical Management of Spasms
Medical management of spasms should begin at least 1 month before surgery. Patients should be given antispasmodic medication and followed to observe any side effects. Some common medications used in clinical practice for control of spasms are discussed below.
6.4.1 Baclofen (Lioresal®)
Baclofen (Lioresal®) is a gamma-aminobutyric acid derivative. An analog to a natural neurohumoral transmitter in the central nervous system that causes presynaptic depolarization, baclofen affects presynaptic hyperpolarization. Its major side effects are anxiety, depression, and sedation. Precautions should be taken when prescribing the drug to the elderly group. Some patients develop coma secondary to baclofen. The medication should be started in small doses and increased gradually. In addition, abrupt discontinuation of the medication may cause side effects. The usual dose of baclofen is 20–25 mg four times per day.
6.4.2 Diazepam (Valium®)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








