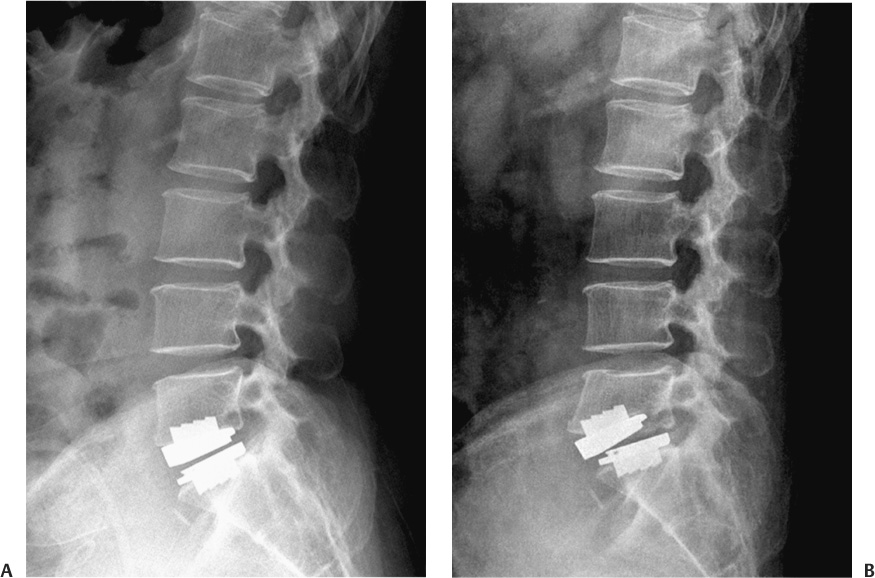
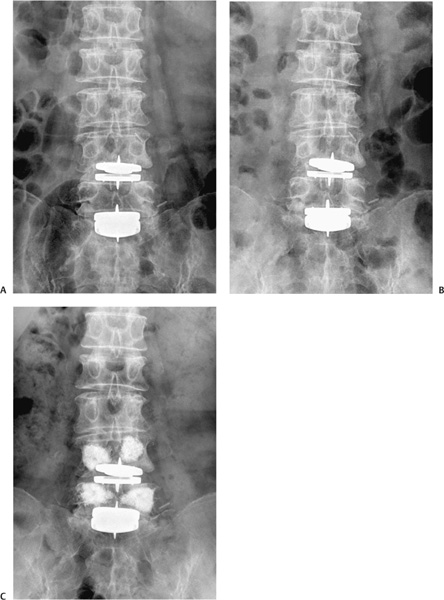
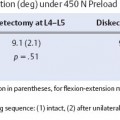
29 Migration of Polyethylene Core Device Migration, Dislocation, or Subluxation Fracture of the Vertebral Body Cerebrospinal Fluid Leakage and Root Injury Polyethylene Wear and Osteolysis Recent successful clinical results of lumbar disk arthroplasty have provoked widespread enthusiasm. The early- and intermediate-term clinical results of total disk replacement (TDR) were promising.1–15 Early results of prospective randomized studies comparing TDR with spinal arthrodesis have shown that TDR is doing as well or better than fusion.16–20 But the complications of TDR reported so far are neither rare nor minor in their potential severity. The incidence of complications even with experienced surgeons are not negligible and it is expected that the incidence will increase if TDR is widespread and done by less experienced surgeons.21 Furthermore, some of the reported complications are significantly dangerous and difficult to deal with.22 Therefore, it is worth appreciating all of the reported complications in this early period of enthusiasm to be aware of the real advantages and disadvantages of lumbar TDR and to avoid complications, if possible, when it is adopted in one’s own practice. This chapter discusses the complications of lumbar disk arthroplasty that are not related to surgical approach. Subsidence of the prosthesis is one of the common complications of TDR. It is generally regarded as a late complication of disk arthroplasty and Cinotti et al4 stated that subsidence occurred in patients who had an undersized prosthesis. In our series, however, subsidence occurred in the early postoperative period in relation to a fracture of the vertebral body (Fig. 29–1) or in patients with osteoporosis (Fig. 29–2). Marked subsidence and the resultant change in the configuration of the prosthesis could make the polyethylene core extrude. Because the extruded core may damage the great vessels that lie in front of the vertebral column, the prosthesis should be removed when the subsidence is identified in the immediate postoperative period or the configuration of the prosthesis is distorted significantly. However, in cases where the subsidence is not significant, reinforcement of the vertebral body with polymethyl methacrylate (PMMA) can prevent further sinking of the prosthesis (Fig. 29–2C). Technical error may be one cause of the subsidence. End plate preparation should be carefully done to make the plates of the prosthesis parallel because obliquity in the coronal plane may cause subsidence (Fig. 29–2A). The prosthesis should be positioned in the center of the coronal plane of the disk space to maintain the coronal balance of the spinal motion segment. Advanced segmental scoliosis preoperatively should be regarded as a relative contraindication of TDR because it is difficult to restore the scoliotic segment with an artificial disk. A patient with significant osteoporosis also should be excluded from TDR. In patients who have osteoporosis and refuse to accept fusion, augmentation of the vertebral body with PMMA may be a possible solution. There has been a successful report of concomitant augmentation of the vertebral body with PMMA in a patient with osteoporosis who underwent TDR,23 but long-term data are needed to prove its long-term efficacy. Delayed subsidence several years after the successful implantation of the prosthesis is another concern. When the vertebral body becomes osteoporotic as the patient ages, because of the discrepancy of the strength between bone and prosthesis, the prosthesis could subside. Although some investigators presumed that the porous-coated end plates (titanium and hydroxyapatite) would improve biological fixation of the metal plates to the vertebral bodies,24 it is uncertain that it could prevent late subsidence of the prosthesis. Figure 29–1 (A) Fifty-eight-year-old female. Lateral radiograph taken postoperative day 1 showed proper positioning of the implant. (B) On postoperative day 6, she felt severe back pain and radiography revealed subsidence of the implant with a transverse fracture of the L5 vertebral body. The prosthesis was removed and anterior lumbar interbody fusion was done. (Courtesy of Dr. Byung-Joon Kong.) There was a case of migration of the polyethylene core reported in the ProDisc series and it was attributed to technical fault.19 With the SB Charité (DePuy Spine, Raynham, MA) it occurred at the L5–S1 level where there was a large lumbosacral angle and hyperlordosis with a large distance between the two vertebral end plates anteriorly and a narrow posterior disk space. In such a case, David24 proposed to use the prosthesis with a more acute angle and place it more posteriorly. In our experience of 620 TDR cases, we have encountered one case of extrusion of the polyethylene core with resultant subluxation of the upper plate of the ProDisc (Synthes, Inc., West Chester, PA). In our opinion, the extrusion of the core is closely related to surgical technique. It is important to see that the core is securely positioned after the insertion. With the ProDisc, it is easy to see if the core is properly placed because the anterior margin of the core is at the same level of the device plates and it should not protrude over the edges of the plates of the prosthesis. With the SB Charité, it is better to confirm the position of the core with fluoroscopy because there is a metallic marker around the polyethylene core. Device migration or dislocations were reported in the study of previous models of the SB Charité (Charité I and Charité II)7,25 but with the SB Charité III, the incidence of migration or subluxation has decreased.4,5 With the ProDisc, though, there is no reported device migration or subluxation in the literature.8,11,12 We experienced a case of device subluxation in our ProDisc series. One reason that the ProDisc showed no incidence of device migration or subluxation may be that it has a high keel on the plates that gives more solid fixation in the immediate postoperative period than does the SB Charité. Fracture of the posterior corner of the vertebral body is a well-known complication of the SB Charité replacement (Fig. 29–3). The SB Charité has spikes on the anterior and posterior margin of the plates and these spikes can cause fracture of the posterior lips of the vertebral body during insertion of the prosthesis. It is better to prepare the posterior portion of the vertebral end plates adequately for smooth insertion of the prosthesis with a high-speed drill or a curette. It was also recommended that once the polyethylene core has been inserted, the prosthesis should not be hammered to be placed posteriorly.24 If the fracture of the posterior lip of the vertebral end plate is identified immediately after the surgery and the patient has symptoms of neural compression, the bony fragment should be removed by either an anterior or a posterior approach. We prefer the posterior approach because it can allow removal of the bony fragment compressing the thecal sac and root without the need to manipulate the prosthesis. Figure 29–2 (A) Sixty-two-year-old female. The immediate postoperative anteroposterior plain radiograph showed unparallel plates of L4–L5 prosthesis. (B)
Complications of Lumbar Disk Arthroplasty
Early Complications
Subsidence
Migration of Polyethylene Core
Device Migration, Dislocation, or Subluxation
Fracture of the Vertebral Body
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 Early Complications
Early Complications Late Complications
Late Complications Conclusion
Conclusion