CHAPTER 7 Claw Hallux Deformity
CLAW HALLUX DEFORMITY SECONDARY TO A COMPARTMENT SYNDROME
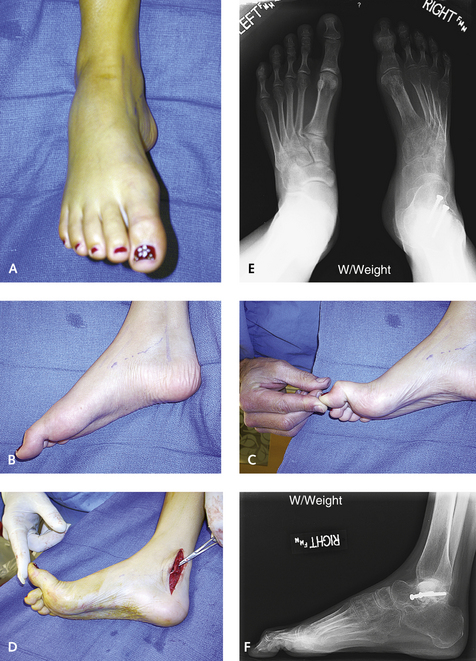
I have attempted various soft tissue releases and ultimately have come to the conclusion that the only way this deformity can be repaired is by completely releasing the sesamoid complex. The approach is through a medial incision similar to that for a sesamoidectomy, and the branch of the medial plantar nerve is identified and retracted. The abductor tendon as well as the volar plate is now cut, identifying the flexor hallucis longus. Once the flexor hallucis is retracted, then the volar plate ligament is cut completely, allowing the sesamoids to retract proximally. The hallux is then passively dorsiflexed. At this time, at least 45 degrees of passive dorsiflexion with the ankle in neutral should be possible. If this is not present or if the hallux is starting to contract at the IP joint, then a lengthening or transfer of the flexor hallucis longus needs to be performed. It is preferable to perform this lengthening proximally, proximal to the medial malleolus either through a fractional lengthening at the musculotendinous junction or by a standard Z-lengthening of the tendon. If a step-cut Z-lengthening is performed, at least 60 degrees of passive dorsiflexion of the hallux must be achieved, because some recurrent contracture is to be expected postoperatively. Once the volar plate has been completely released, the effect of the contracture on the interphalangeal joint must be observed. Is this is a fixed contracture, or is there a passive tenodesis effect of the FHL that is eliminated with plantar flexion of the ankle? In order to determine this, plantar flex the foot and assess the amount of dorsiflexion that occurs through the interphalangeal joint. If the IP joint can be straightened completely with the foot plantar flexed but flexion of the hallux at the IP joint is observed with the foot in neutral or dorsiflexion, then a tenodesis effect is present. If a fixed flexion contracture is present, then an arthrodesis of the interphalangeal joint can be performed or the FHL transferred into the base of the proximal phalanx of the hallux (Figure 7-1).
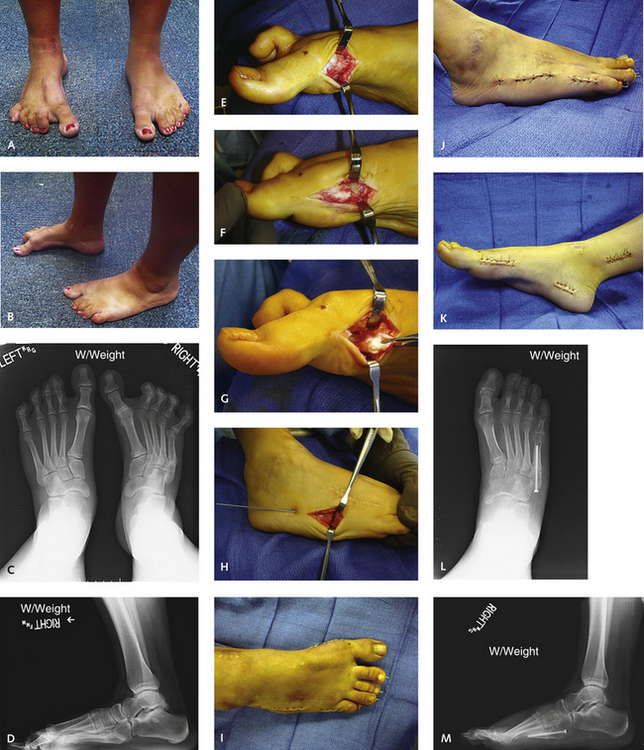
In many patients with deformity secondary to injury, the contracture responsible for clawing of the hallux is caused by fibrosis of the intrinsic musculature. This is far more difficult to treat, and although the hallux will function, it will never be normal. Most affected patients present with a fixed flexion at the MP joint, with some remaining function and flexibility at the IP joint. I have tried numerous procedures to release the hallux MP joint contracture and have found that a complete release allowing the sesamoid complex to retract proximally is the only realistic option. This application is well illustrated in Figure 7-2, in which the patient’s severe forefoot deformity was the result of a compartment syndrome that developed after an ankle arthroscopy. Very fixed flexion and adduction deformity of all of the MP joints is evident on the preoperative weight-bearing radiographs. A good aesthetic and functional result was achieved with extensive surgical release as described.