CHAPTER 1 Chevron Osteotomy
INDICATIONS
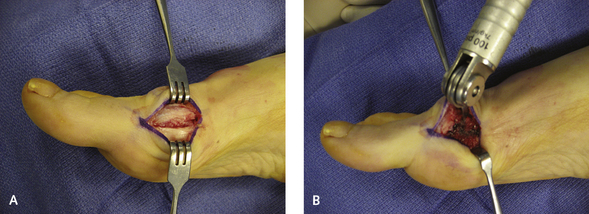
The incidence of avascular necrosis of the metatarsal head does not increase when a soft tissue release is performed simultaneously with the osteotomy. Avascular necrosis of the metatarsal head typically results when excessive periosteal stripping is performed along the dorsal lateral metatarsal neck, which really does not need to be exposed. The osteotomy can be performed in conjunction with a closing wedge osteotomy of the hallux proximal phalanx (Akin osteotomy) for patients in whom the distal metatarsal articular angle (DMAA) is abnormal (Figure 1-1). It is preferable, however, to perform a biplanar chevron osteotomy if any doubt remains about the congruency of the articulation achieved with a closing wedge osteotomy. In geometric terms, the improvement obtained in the distal angulation between the first and second metatarsals will correspond to the magnitude of the lateral shift. It is stated that a 1-degree improvement in angulation will take place with a 1-mm shift of the metatarsal. Although this dictum implies that a deformity greater than 14 degrees cannot reestablish the alignment, such limitation is not supported in clinical practice if a soft tissue release is performed.
APPROACH TO A STANDARD CHEVRON OSTEOTOMY
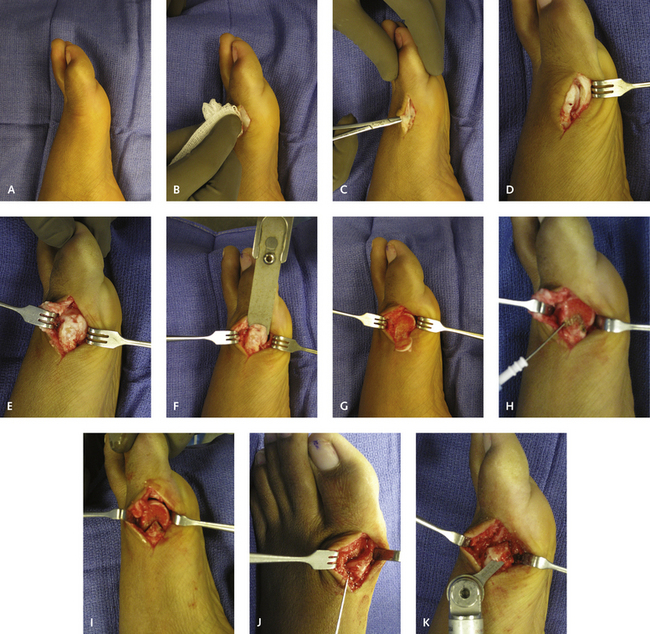
An incision is made medially at the junction of the dorsal and plantar skin, extending proximally for 3 cm from the flare just distal to the metatarsophalangeal joint. This incision is far safer, with more predictable results, than a dorsally based approach, which endangers the nerve and is associated with increased risk for an extension contracture. The incision is deepened through subcutaneous tissue. The soft tissues are dissected carefully to identify the terminal medial cutaneous branch of the superficial peroneal nerve, which is then dorsally retracted (Figure 1-2). It is easier to free the nerve with a hemostat, rather than with a knife or scissors.
The osteotomy is planned with use of a cautery to mark the apex, approximately 8 mm proximal to the articular surface. I prefer a standard cut at a 60-degree angle, with the dorsal and plantar limbs of the osteotomy equidistant. Although alternative limbs of the osteotomy have been described, use of such alternatives offers no advantages, requires more dorsal exposure and dissection, and is likely to result in further metatarsal shortening. For exposure of the dorsal surface of the metatarsal, the soft tissue is dissected dorsally with limited subperiosteal dissection. Visualizing the dorsal-lateral metatarsal is unnecessary, and only the dorsal and medial aspect of the first metatarsal neck is exposed. Care should be taken not to strip any periosteum on the plantar or dorsal surface more proximal to the level of the osteotomy. A saw blade is used for the osteotomy and aligned perpendicular to the axis of the planned limbs of the osteotomy. It is essential not to overperforate the soft tissues laterally; the saw blade should penetrate the lateral cortex only. In cases with a long first metatarsal, slight shortening of the metatarsal may be advantageous, and the saw blade can be oriented or angulated slightly proximally (Figure 1-3). The same concept applies with a short metatarsal, in which case any shortening must be avoided.