(1)
Department of Orthopaedics and Sports Medicine, University of Washington, 3950 Montlake Boulevard NE, Room 148, Seattle, WA, USA
(2)
Orthopedic Surgery, Cartilage Study Group, Hospital for Special Surgery, 535 E 70th Street, New York, NY, USA
(3)
Weill Cornell Medical College, New York, NY, USA
Abstract
Articular cartilage lesions are commonly associated with anterior cruciate ligament (ACL) tears and are often encountered at the time of ACL revision surgery. Concomitant cartilage lesions can affect outcome after ACL revision and should be addressed at the same time. We discuss different repair strategies for cartilage injury and their implementation in the context of revision ACL reconstruction.
Introduction
The anterior cruciate ligament (ACL) in the knee is commonly injured with an incidence reported between 36.9 and 80 per 100,000 person-years [1–3]. In the young and active patient population, ACL reconstruction is performed to restore knee stability, protect against future meniscal injury and return patients to pre-injury activity levels. It is estimated that between 2 and 6 % of primary ACL reconstructions will fail [4]. Many of these patients ultimately will undergo revision ACL surgery.
Cartilage injuries associated with ACL tears are common. Concomitant cartilage abnormalities at the time of revision ACL reconstruction occur at a rate between 10 and 70 % [5–18]. This represents a significant difference compared to cartilage lesions encountered at the time of primary ACL reconstruction [19]. Although the majority of these cartilage lesions do not play an important role in overall knee joint stability, in the ACL deficient knee, left untreated they represent potential for poor clinical outcome after revision ACL surgery [7, 17, 20].
ACL deficiency is a contraindication to cartilage repair therapies [21]. The persistent knee instability leads to a high likelihood of repair failure due to increased shear stress on the articular cartilage of the knee. Therefore, revision of a failed ACL reconstruction is important not only from the standpoint of ligament stability and return to athletic participation but as protection for the cartilage repair. The primary goal of surgical intervention should be directed toward the reestablishment of joint stability and congruity through ligament reconstruction coupled with cartilage restoration strategies when indicated. The purpose of this chapter is to discuss the approach to cartilage repair surgery in the setting of revision ACL reconstruction.
“Bone Bruise” and Articular Cartilage Injury Associated with ACL Rupture
Patients with ACL deficiency are at increased risk for future cartilage problems and posttraumatic osteoarthritis compared to healthy individuals. This process of articular cartilage degeneration may be independent of ACL status, with several studies recently showing continued cartilage degradation despite stable ACL reconstruction [22, 23].
The significance of the bone marrow edema pattern that is commonly associated with ACL injury remains poorly understood. These “bone bruises,” areas of increased signal intensity best visualized on the T2-weighted MRI images (Fig. 18.1), are present in approximately 80 % of ACL tears [24, 25]. This bone marrow edema pattern represents evidence of transchondral injury that results from the impact that occurs during the pivot-shift phenomenon as the posterolateral aspect rotates forward and the tibia impacts the anterolateral femur. These lesions are most commonly seen after acute ACL ruptures on the posterolateral tibia and the anterolateral femoral condyle. Studies that followed these lesions on MRI over time have shown that the bone marrow edema improves with time. However, the damage to the overlying cartilage is irreversible [26–28].


Fig. 18.1
Sagittal fat-suppressed T2-weighted MRI sequence demonstrates typical bone marrow edema pattern (“bone bruise”) after acute anterior cruciate ligament tear
Histologically, these areas of articular cartilage have been shown to undergo chondrocyte and matrix degeneration [29]. This has been corroborated by Potter et al. using MRI studies to follow patients with isolated ACL tears over time [22]. Their study identified acute cartilage damage overlying the areas of bone bruising at the time of injury as well as ongoing cartilage loss with time despite undergoing ACL reconstruction. Unfortunately, the investigators found that the rate of cartilage loss accelerated at 5–7 years after initial injury and was not limited to the lateral hemijoint where the original impaction occurred. Instead, the medial and patellofemoral compartments showed the highest rate of cartilage loss.
Clinical Approach
Surgical decision-making for the treatment of focal cartilage lesions in the setting of ACL deficiency should proceed in a logical fashion and should not be altered by the decision-making regarding the ACL. Once ACL reconstruction or ACL revision reconstruction is planned, the approach to the concomitant cartilage lesion should not differ from that of an isolated lesion. Thus, the surgical indications remain unchanged and include:
1.
Isolated chondral or osteochondral lesion of the knee condyles, trochlea, or patella
2.
Symptoms of knee dysfunction (pain, recurrent effusion, mechanical symptoms)
3.
Normal or correctable knee ligament stability
4.
Normal or correctable alignment
5.
Functional meniscus tissue (>50 % native meniscal volume)
Contraindications to cartilage repair:
1.
Degenerative knee osteoarthritis
2.
Systematic inflammatory disorders (e.g., rheumatoid arthritis)
3.
Collagen or vascular disorders
4.
Obesity
5.
Chronic use of immunosuppressive medication (e.g., corticosteroids)
The surgeon should have a clear approach to articular cartilage injuries of the knee and must take into account both patient and surgeon factors in the decision-making process. The first step is to identify the factors that will affect treatment on the patient’s side. This starts with categorization of the likely etiology of the chondral defect. Most commonly, cartilage defects occur secondary to traumatic injury, chronic degeneration or an abnormality in the underlying bone such as avascular necrosis (AVN) or osteochondritis dissecans (OCD). In the setting of an ACL deficient knee, most commonly the cause is traumatic, but this is not always the case. Therefore, careful thought must be given to the etiology in order to address this in advance of or concomitant with ACL reconstruction.
The next consideration is the characteristics of the cartilage lesion which should include:
1.
Size
2.
Location
3.
Grade
4.
Lesion morphology
It is important to obtain as much of this information as possible preoperatively as this impacts surgical decision-making. This is best achieved through the use of cartilage-sensitive MRI imaging. However, sometimes the true nature of the lesion will not be apparent until it is visualized intra-operatively and the surgeon must be prepared for this possibility.
During the evaluation process, one must not forget to determine the global condition of the knee and the lower extremity. If there are abnormalities that could jeopardize the success of the cartilage repair these will need to be addressed. Ligament deficiencies should be corrected by repair or reconstruction. Any meniscus tear(s) should be appropriately debrided, repaired or replaced with allograft transplantation. Limb malalignment may need to be corrected using an osteotomy and most importantly, the patient should have preserved articular cartilage surfaces (Grade 2 or better) throughout the remainder of the joint.
Special note should be made concerning multiple focal cartilage defects. Although this is not an absolute contraindication to multiple repairs, the surgeon should proceed with caution in these situations as this likely represents early generalized cartilage degeneration. One must pay particular attention to bipolar (i.e., opposing condyle-plateau or patella-trochlea) lesions which have been noted in studies to fare poorly when they have been treated using osteochondral allografts [30, 31].
Preoperative Planning
Prudent preoperative planning for cartilage repair must also take into consideration patient-related characteristics. These include:
1.
Age
2.
Body mass index (BMI)
3.
Level of demand
4.
Systemic conditions of disease
5.
Patient functional needs
6.
Patient expectations
7.
Ability to comply with rehabilitation
The age and BMI have importance when deciding on treatment options as there have been studies that demonstrated a negative clinical effect of increasing age and patients with higher BMIs undergoing specific cartilage restoration techniques [32, 33]. The level of demand of the patient and functional need should also be considered as these have implications for treatment decisions. The elite collegiate or professional athlete will place a vastly different demand on his knee than the middle-aged “weekend warrior” and so different treatment regimens should be considered in those situations.
One additional aspect of preoperative planning involves assessment of the surgeon’s own characteristics. This refers to the insight of the surgeon into his surgical skills and abilities with the many varied techniques that have evolved for cartilage repair and regeneration. The different surgical treatments can vary in their degree of technical difficulty, which must be taken into consideration along with the surgeon’s level of experience and comfort with each procedure.
Patient Evaluation
The patient evaluation begins with a thorough history and physical examination. Specific attention is given to previous treatments, especially in regards to previous ACL reconstruction, including graft type and concomitant intra-articular findings at the index surgery. The mechanism of reinjury should be sought and the etiology of ACL graft failure should be pursued. Obtaining arthroscopic images from the previous surgeries can be helpful in understanding the status of the cartilage at the time of the index reconstruction and for future preoperative planning.
The initial imaging studies should include plain radiographs of the knee, including weight-bearing anteroposterior (AP), 40° posteroanterior (PA), lateral, Merchant’s view. The bilateral standing hip-knee-ankle AP view can also be helpful in determining overall limb-alignment. Further imaging with cartilage-sensitive MRI, which is the imaging modality of choice in these cases, is essential. This allows the surgeon to evaluate the previous ACL graft (or lack thereof) and assesses the meniscus as well as articular cartilage for any concomitant abnormalities.
Special attention must be paid to the patient with patellofemoral joint cartilage lesion(s) in the setting of a previous ACL reconstruction. In this case, it is not uncommon for pain and/or mechanical symptoms stemming from the patellofemoral articulation to be reported by the patient as a subjective history of knee instability. This subtlety must be discerned by the clinician by detailed history taking, a thorough knee examination and MRI evaluation for the status of the previous ACL graft and the status of the cartilage surfaces.
Current Cartilage Repair Strategies
Articular cartilage injuries and their treatment remain difficult problems in orthopaedics. The broad categories of treatment options available to the surgeon include:
1.
Mechanical debridement
2.
Intrinsic repair enhancement: marrow stimulation
3.
Whole tissue transplantation
(a)
Osteochondral autograft (mosaicplasty)
(b)
Osteochondral allograft
4.
Cell-based repair
5.
Cell and scaffold-based repair
6.
Scaffold-based repair
Mechanical Debridement
This involves the arthroscopic debridement of any chondral flaps and general lavage of the knee joint without any attempt to fill the cartilage defect. This is used as a palliative therapy as it serves to remove the potential mechanical and biochemical sources of pain but does not repair the lesion(s). This procedure is indicated in the setting of early generalized cartilage degeneration where other repair strategies are contraindicated.
Marrow Stimulation
The goal of marrow stimulation, or microfracture, is recruitment of marrow-based stem cells to the site of the cartilage defect by perforation of the subchondral plate at the base of the lesion. This is a simple and low-cost option and can be used in small and large lesions. This technique requires a stable blood clot to form and fill the defect. The clot contains cells and growth factors that ultimately fill the defect with fibrocartilage. The disadvantages of this technique include the lengthy postoperative rehabilitation process and that microfracture achieves fibrocartilaginous healing which is structurally inferior to hyaline cartilage.
The success of microfracture has been shown to be dependent on adequate fill of the defect and this is dependent on good surgical technique [34–36]. Preparation of a well-contained lesion at the time of surgery is critical and involves the debridement of the surrounding zone of cartilage injury back to a healthy rim of cartilage that will serve to “shoulder” the clot. Debridement of the calcified cartilage layer found at the base of the lesion also facilitates stable clot adhesion and is important for success of this technique [37]. Also, the perforations into the subchondral bone must be of sufficient depth to reach marrow elements and visualization of fat-droplets at the time of microfracture ensures that this has been achieved (Fig. 18.2).
Fig. 18.2
(a, b) Demonstrate the creation of a well-shouldered lesion to achieve a stable base for filling of the defect with a clot and adhesion of the clot after microfracture. The calcified cartilage layer at the base of the lesion must be removed to allow clot adhesion. (c, d) Show that channels must be of sufficient depth to ensure penetration of the subchondral plate and communication with the marrow (reproduced with permission from Bedi A, Feeley BT, Williams RJ III. Management of articular cartilage defects of the knee. J Bone Joint Surgery Am. 2010;92:994–1009)
Postoperatively, patients are maintained non-weight bearing for a minimum of 6 weeks as early weight bearing can lead to collapse of the subchondral plate or flattening or dislodgement of the clot. Continuous passive motion (CPM) from 0 to 60° is initiated immediately and continued for the first 6 weeks. CPM should be performed for 6–8 h per day and the flexion may be increased 10° per day until full motion is achieved. Isometric exercises and dynamic quadriceps strengthening is started 1 week after surgery under the guidance of a physical therapist and water exercises and stationary bicycle therapy is initiated at 2 weeks if range of motion allows. Pivoting and jumping activities are prohibited until a minimum of 4 months after surgery. Running is restricted until 6 months after surgery and return to high-level sports is permitted at 8–12 months depending on quadriceps and core strength.
Steadman and his colleagues have reported success with microfracture for full-thickness traumatic cartilage defects at an average follow-up period of 11 years [33]. Mithoefer and his colleagues also showed that 67 % of 48 patients had good to excellent response who underwent microfracture for lesions between 1 and 4 cm2. In their analysis, the authors noted that lower BMI was a predictor of better outcomes and that the initial clinical response deteriorated with time in 47 % of elite athletes [32, 38]. Several other studies have investigated microfracture for cartilage lesion in elite professional athletes in football and basketball and reported over 70 % return to play postoperatively [39, 40].
Whole Tissue Transplantation
Osteochondral Autograft Transfer/Mosaicplasty
Osteochondral autograft transfer, also known as mosaicplasty, is used to treat focal full-thickness cartilage defects most commonly occurring from traumatic etiologies and it can also address lesions associated with significant bone loss such as OCD. This technique involves the transplantation of multiple small cylindrical osteochondral plugs (forming a mosaic) into a larger sized cartilage defect from the less weight-bearing aspects of the knee joint. The advantages of this procedure include the fact that viable hyaline cartilage is directly transplanted into the defect, the grafts are press-fit and do not require additional fixation, the rehabilitation process is relatively short, and the procedure is performed in a single-stage either arthroscopically, or arthroscopically aided with a mini-arthrotomy.
The main disadvantages of the procedure are the donor site morbidity and the limitations in terms of size of defects that this technique can address due to the autologous nature of the donor plugs (the osteochondral plugs are taken from the periphery of the patellofemoral joint and/or the area adjacent to the intercondylar notch) (Fig. 18.3). The indication for mosaicplasty is a focal full-thickness cartilage lesions ranging from 1 to 5 cm2. Osteochondral transfer is more technically demanding than other techniques such as microfracture and usually requires an open arthrotomy. Other limitations include the persistence of gaps in the mosaicplasty, graft subsidence with weight-bearing, and donor-recipient site mismatch in terms of cartilage orientation, thickness and mechanical properties [41].
Fig. 18.3
(a) Schematic drawing demonstrating the autologous osteochondral transplantation technique. (b) The donor region along the trochlear margin can be accessed through a small arthrotomy and visualized with the knee in extension. (c) Flexion exposes the recipient chondral defect through the same exposure and allow placement of grafts in the desired configuration to fill the lesion (reproduced with permission from Bedi A, Feeley BT, Williams RJ III. Management of articular cartilage defects of the knee. J Bone Joint Surgery Am. 2010;92:994–1009)
Several studies of mosaicplasty have shown good clinical success in the treatment of Outerbridge grade III and IV lesions [42, 43]. Hangody showed clinical success with this technique at long-term follow-up on full-thickness cartilage lesions on the femoral, tibial and patellofemoral articulations with minimal donor site morbidity [44]. Nho et al. performed a retrospective review of isolated patellar chondral lesions treated with this technique and showed a significant clinical improvement in IKDC score and MRI evidence of complete or near complete fill in all plugs at final follow-up [45]. Ozturk and his colleagues showed similar results using mosaicplasty in a series of 19 patients and reported 85 % good to excellent results at a mean follow-up of almost 3 years [46].
When compared with microfracture, osteochondral autograft transfer has shown better clinical results and biopsy specimens taken from both groups at second-look arthroscopy demonstrated better repair with osteochondral autograft. The authors of the study concluded that the osteochondral autograft transplantation was superior to marrow stimulation for patients under the age of 40 years [47].
Osteochondral Allograft Transplantation
This procedure entails the transplantation of a cadaver graft into the cartilage lesion. As the donor graft can be tailored to the size, location and depth of the cartilage defect, there is improved fit and fill of the plug when compared to mosaicplasty. As with mosaicplasty, this procedure is performed arthroscopically assisted with a mini-arthrotomy. Using specialized proprietary instrumentation, a cylindrical osteochondral plug is obtained from the allograft (Fig. 18.4), preferably from the same location of the same hemijoint such that the contour and shape matches the donor site. The recipient site is prepared using a cylindrical punch which is slightly smaller in diameter which allows for press-fit fixation without additional hardware.
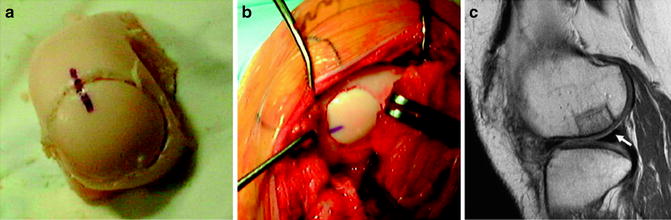
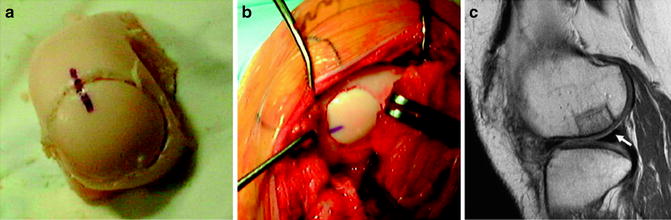
Fig. 18.4
(a) Harvesting of an osteochondral allograft dowel from a hemicondylar specimen with the size and radius of curvature matched to the recipient. (b) Implantation with circumferential flush congruity at the recipient site for the treatment of an osteochondritis dissecans lesion of the femoral condyle. Corresponding pen marks are made at the 12, 4, and 8 o’clock positions in an effort to optimally match the orientation and surface congruity between the donor graft and the recipient defect. (c) Sagittal fast spin-echo magnetic resonance image made at 24 months after implantation of the osteochondral allograft. There is excellent lesion fill and congruency with the adjacent native cartilage interface. The graft demonstrates articular cartilage signal (arrow) that is isointense compared with the native hyaline cartilage (reproduced with permission from Bedi A, Feeley BT, Williams RJ III. Management of articular cartilage defects of the knee. J Bone Joint Surgery Am. 2010;92: 994–1009)
There are several advantages of allograft transplantation including the ability to address larger size cartilage defects with a single osteochondral plug which better reproduces the contour of the surrounding cartilage, no donor site morbidity, and the surgery can be performed in a single-stage in combination with the ACL reconstruction. Concerns with this technique include high cost and donor tissue availability, the rare possibility of disease transmission, and graft rejection [48].
A number of investigations of osteochondral allograft transplantation have shown durable and reliable clinical outcomes for the treatment of posttraumatic cartilage injuries as well as OCD [30, 31, 49, 50]. Several studies have shown over 80 % success using this technique for isolated unipolar full-thickness cartilage lesions up to 8 cm2, but much poorer results were noted in patients who had allograft transplantation for the treatment of bipolar lesions, or who had more systemic derangement of the knee joint, including osteoarthritis, inflammatory arthritis and limb malignment [30, 31




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








