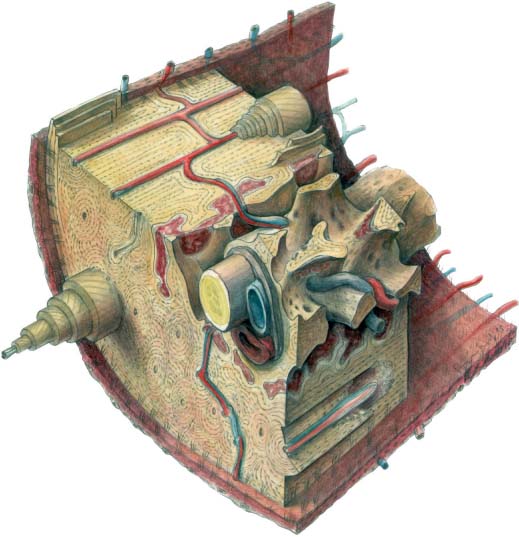
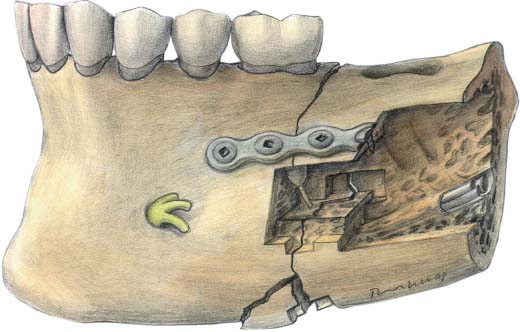
4 Bone Repair and Fracture Healing The structure of facial bone is determined by its material properties and by its mechanical role. The bone marrow cavity, the cortex, and the spongiosa of the mandible and the midface are similar in their material composition. Their major difference is in the geometric distribution of the bone. The midfacial skeleton consists of thin laminae that provide an increased surface-area to bone-volume ratio as compared with the mandible. Consequently, the closer proximity of blood vessels provides a superior supply of nutrients and thus promotes an increased healing rate of the midfacial bones. Bone is a dynamic tissue, constantly undergoing resorption and remodeling (Schenk, 1992). The cell types of which it is composed consist of osteoblasts, osteocytes, and osteoclasts (Fig. 4.1). Osteoblasts are derived from pluripotential precursor cells. They produce osteoid, the organic matrix of bone, which is transformed into calcified bone. A layer of 1 µm of osteoid may be produced per day, followed by a maturation phase of 10 days before calcification. The microscopic structure of osteoid is different in woven and lamellar bone. In woven bone the collagen fibrils are randomly orientated and have a felted texture. In lamellar bone they are arranged in parallel bundles. Woven bone mineralizes immediately after osteoid deposition. In fracture healing, woven bone is transformed into lamellar bone. Fig. 4.1 Normal bone structure. Fig. 4.2 Three windows in a mandibular fracture with miniplate osteo-synthesis on the tension side. This shows indirect bone healing in the window on the inferior border of the mandible with the mobile fragment; direct bone healing in the window of the lateral cortex of the mandible by contact healing after perfect and anatomical reduction; direct bone healing in the window of the inner cortex of the mandible by gap healing. Osteocytes are derived from osteoblasts. Sometimes osteoblasts can stop producing osteoid. They transform into osteocytes, which are connected with the deeper osteocyte cell layers. The osteocytes lie between the concentric lamellae. Osteoclasts are multinucleate giant cells derived from mononuclear macrophages. Osteoclasts have a specialized role of bone breakdown. This activity is limited to How-ship lacunae, which are small subcellular chambers with a low pH. The pH is maintained by hydrochloric acid, which dissolves the mineral. The organic matrix is degraded by proteases and collagenases. Osteoclasts are able to resorb 50–100 µm of bone per day. Osteons are cylindrical vascular tunnels formed by an osteoclast-rich tissue (haversian canal). They contain pluripotential precursor cells and endosteum known as the cutting cone. The bone removed by the cutting cone is replaced by osteoblast-rich tissue, known as the closing cone. This forms concentric layers of lamellar bone which surround the vascular haversian canal. Volkmann canals also contain nutritional vessels arising from the periosteal and endosteal bone surface, which connect with the haversian vessels within the osteons (Schenk and Willenegger, 1964). The size of the osteonal transport system is 100 µm, which limits the width of an osteon to approximately 200 µm. The mean width of a lamella is 3–7 µm (see Fig. 4.1). The three most important conditions necessary for bone formation and bone mineralization are pluripotential precursor cells, ample blood supply, and mechanical rest (Pauwels, 1940).
Structure of Facial Bone
Fracture Healing
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree