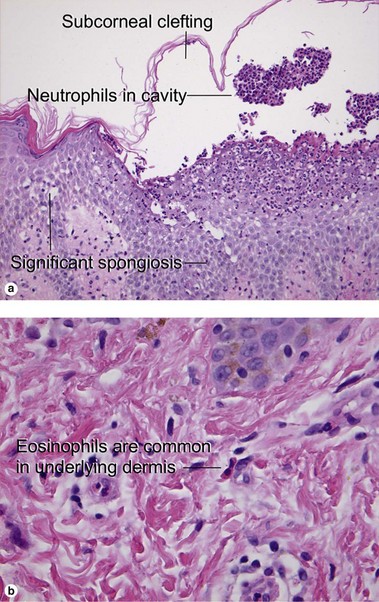
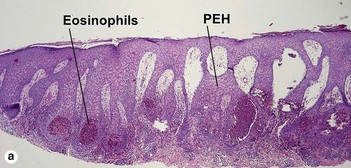
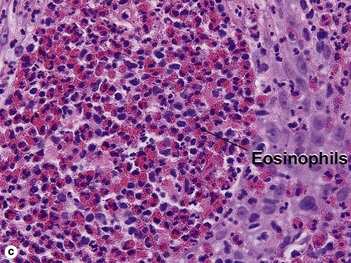
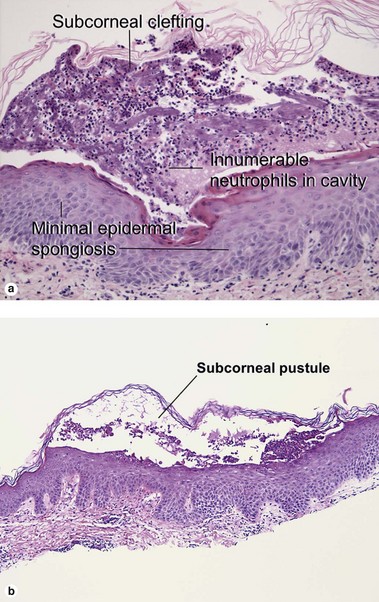
Chapter 9 Pemphigus foliaceus is a subcorneal vesiculobullous disorder caused by autoantibodies directed at an intercellular keratinocyte adhesion protein, desmoglein 1 (160 kD). The disease usually presents with superficial crusted erosions upon the face and upper trunk. The superficial nature of the blisters makes them fragile and most patients lack intact bullae. Fig 9-3 (a) Subcorneal pustular dermatosis. (b) “Subcorneal pustular dermatosis” type of IgA pemphigus Cases of subcorneal pustular dermatosis with intercellular deposition of IgA have been reclassified as IgA pemphigus. Subcorneal pustular dermatosis may represent a subclass of pustular psoriasis, although mitotic figures within the underlying epidermis, common to psoriasis, are not identified in subcorneal pustular dermatosis. The classic patient is an older woman with annular or polycyclic lesions of the trunk or groin with pustules at the periphery. Acute generalized exanthematous pustulosis is an uncommon reaction to exogenous medications. Beta-lactam antibiotics are most often implicated, but a myriad of drug associations have been described. The presence of eosinophils in the inflammatory infiltrate helps distinguish the condition from pustular psoriasis. Early pustules may be noted in association with hair follicles or sweat ducts. Pemphigus vulgaris is an intraepidermal vesiculobullous disorder caused by autoantibodies directed at an intercellular keratinocyte adhesion protein, desmoglein 3 (130 kD). The disease presents with erosions of the skin and mucosa. Often the disease begins in the posterior oropharynx weeks before cutaneous lesions are noted. Most patients lack intact bullae. Erythematous skin shears away easily when lateral pressure is applied (Nikolsky sign). Hailey–Hailey disease is an autosomal-dominant, inherited disease caused by mutations in the ATP2C1 gene. This gene encodes for a portion of a calcium pump essential for proper keratinocyte differentiation and adhesion. Skin of the intertriginous areas is most prominently affected and yields a clinical appearance likened to “wet tissue paper.” Acantholysis at all levels of the epidermis yields the histologic appearance of a “dilapidated brick wall.” While the disease itself is not immunologically mediated, superinfection of macerated skin by bacteria or yeast may engender an underlying inflammatory infiltrate within the superficial dermis.
Blistering diseases
Subcorneal vesiculobullous disorders
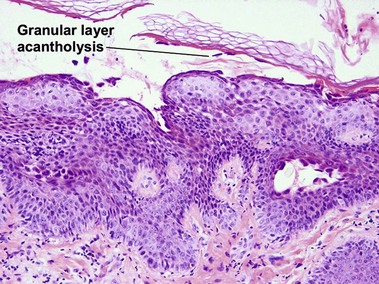
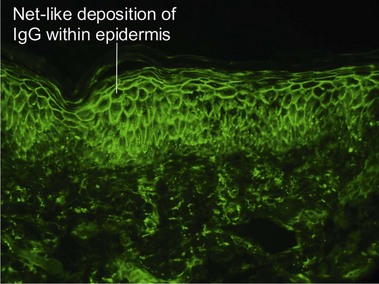
Pemphigus foliaceus
Subcorneal pustular dermatosis (Sneddon–Wilkinson disease)
Acute generalized exanthematous pustulosis
Intraepidermal vesiculobullous disorders
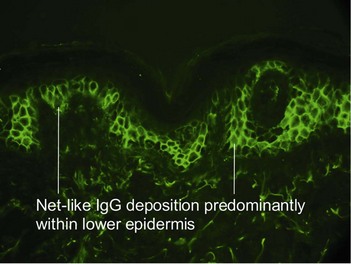
Pemphigus vulgaris
Familial benign chronic pemphigus (Hailey–Hailey disease)