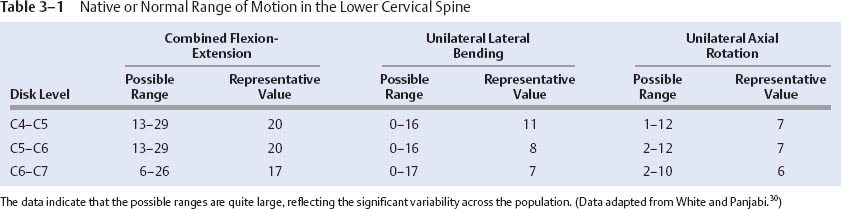
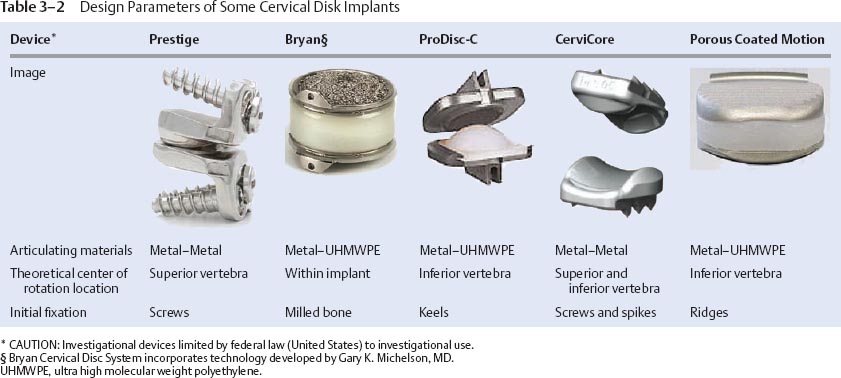
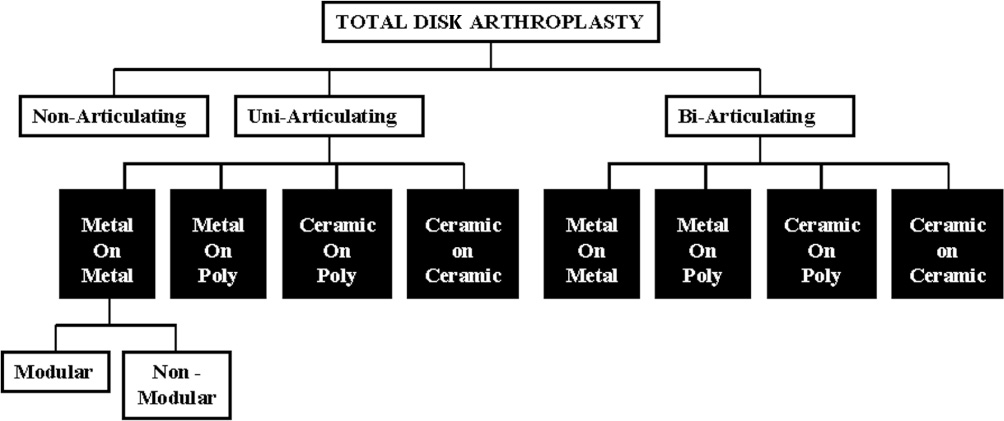
3 Since its description in the 1950s by Cloward1 and Robinson and Smith,2 anterior cervical diskectomy and fusion (ACDF) has become an accepted treatment for cervical myelopathy and disk disease.3 Clinical findings, however, have shown adverse effects of advanced degeneration at the spinal levels adjacent to fusion. The occurrence of adjacent segment degeneration with new, symptomatic radiculopathy varies between 2 and 3% of patients per year on a cumulative basis after ACDF.4,5 An estimated 7 to 15% of patients ultimately require a secondary procedure at an adjacent level.6,7 The increased stress placed on the adjacent segments, particularly the inferior disk, after successful ACDF may increase the rate of future symptomatic disk disease at those segments.8–16 More recently, spine surgeons have become interested in motion-sparing or motion-preserving spinal technologies as alternatives to fusion surgery. The goal of motion preservation is to design instrumentation or effective strategies that target the diseased intervertebral disk. These devices range from repair of local defects, such as annular tears, to complete replacement of the disk. Early clinical experience is growing; however, the biomechanics of cervical disk arthroplasty have not been fully delineated in the literature. This is mainly due to the fact that, although the literature (especially from Europe) is replete with early follow-up studies,17–20 case reports,21,22 survey articles,23–26 and materials consideration with regard to disk arthroplasty designs,27–29 there is a limited number of peer-reviewed publications on the biomechanical aspects of cervical disk replacement. This chapter provides an overview of the current research in disk arthroplasty biomechanics. Cervical radiculopathy refers to pain or motor dysfunction caused by either or both mechanical deformation and inflammation of the nerve roots in the cervical spine. The etiology of radiculopathy can be diskogenic. When conservative management fails to alleviate the pain and neurological deficits caused by disk herniation, the patient is offered the option of surgical decompression of the affected nerves and spinal cord. Cervical decompression is most often accomplished via partial or complete removal of the diseased disk, providing immediate relief of pressure to the spinal cord and associated nerve roots, and treatment with an ACDF. Although ACDF has proven to be a very successful procedure,3 fusion of a relatively mobile spinal segment is not an ideal reconstruction and can potentially lead to deleterious, long-term iatrogenic effects. The goal of disk arthroplasty is to replace the diseased disk while preserving or restoring cervical disk motion at the operated level. The prosthesis is designed to act as an intervertebral body spacer that maintains disk space height and spinal decompression while theoretically reducing the likelihood of accelerated degeneration in adjacent disks through the preservation of normal disk kinematics at the affected disk level. It should also impart stability to the affected area that approximates what is normally seen in the native spine. Lastly, if the disk arthroplasty fails and leads to a painful pseudarthrosis, then the implantation of a disk arthroplasty device should not preclude or significantly complicate a subsequent fusion procedure. Given that the primary aim of the cervical disk device is to maintain motion, it is important to review the ranges of “normal” or “physiological” motion that are typically present at the lower cervical (C4–C7) spinal levels. The most commonly cited source of spinal kinematic data is the classic text of White and Panjabi,30 wherein ranges of motion for combined flexion-extension, one side lateral bending, and one side axial rotation are presented from compilations of many spine researchers. Representative values that fall in the middle of these ranges are also provided and are listed in Table 3–1. All three motion planes exhibit a relatively high degree of mobility at all three lower cervical levels. However, the large disparity that exists in the amount of motion afforded at each level across the general population further complicates the ability to target a specific motion for each arthroplasty design. This finding is evidenced by the large variations in ranges of sagittal, transverse, and frontal plane motions given in Table 3–1. Nevertheless, the goal of most disk arthroplasty designs is to approximate the normal spinal kinematics as closely as possible. The guiding rationale behind these designs is that preservation of motion offers a better clinical outcome than fusion. Many designs have been advocated as replacements for cervical intervertebral disks that consist of either articulating or nonarticulating components constructed from various materials (Table 3–2). Most of these implants consist of metallic or polymeric components or both. A classification system was proposed by the Cervical Spine Study Group to better understand the similarities and differences among these design features26 and is shown in Fig. 3–1. Some devices, by the nature of their geometric design, limit the amount of possible motion in certain planes or do not provide for coincident translation during rotation and are often referred to as constrained or semiconstrained. Other devices, commonly called unconstrained prostheses, rely on the perispinal soft tissue architecture and the inherent compression across the disk space to provide support and restrict the end limits of rotation and translation. The design rationale for many of these implants seeks not only to replicate the rotational kinematics of the cervical spine but also to mimic the physiological path of the center of rotation between adjacent spinal segments. Thus, based largely upon the geometry of the articulating surfaces, either a constrained design has the center of rotation fixed within the body of the implant or in the adjacent inferior or superior vertebral body, or a semiconstrained design provides a variable or changing axis of rotation but not necessarily the physiological instantaneous axis of rotation. Unfortunately, these design differences have had little impact on the overall acute kinematics, and, as discussed later, their effect on the loading mechanics of the spine remains poorly understood. In response to the increasing interest in spine arthroplasty and the current concepts for disk prosthesis design, it is not surprising that the actual kinetic and biomechanical effects that cervical disk arthroplasty imparts on the spine have become more widely reported. The majority of biomechanical studies have used human cadaveric models to compare the spinal range of motion before and after implantation of the device. These studies evaluated several cervical arthroplasty disk designs that are widely available in Europe and that are undergoing investigational Food and Drug Administration (FDA) clinical trials in the United States. The following gives a brief summary of the various studies that have been reported in peer-reviewed journals. Figure 3–1 The Cervical Spine Study Group’s artificial cervical nomenclature allows for classification of the different designs for cervical implants.26
Biomechanical Aspects Associated with
Cervical Disk Arthroplasty
 Design Rationale for Cervical Arthroplasty
Design Rationale for Cervical Arthroplasty
 Peer-Reviewed Biomechanics Literature
Peer-Reviewed Biomechanics Literature
Design Rationale for Cervical Arthroplasty
Peer-Reviewed Biomechanics Literature
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 Conclusions
Conclusions