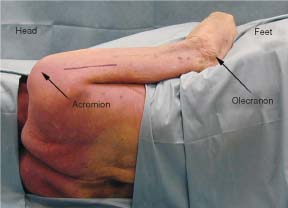
3 The axillary nerve arises from the posterior cord of the brachial plexus distal to the subscapular and thoracodorsal nerves. It is made up of fibers primarily from the C5 and C6 nerve roots. Occasionally, fibers from the C7 nerve root also contribute to the nerve.1 Moving laterally and obliquely the nerve descends behind the axillary vessels and on the surface of the subscapularis muscle. At the region of the subscapularis musculotendinous junction it turns sharply posterior and, along with the posterior circumflex humeral vessels, enters the quadrangular space. It gives off a branch to the shoulder joint capsule prior to entering the space. The nerve then passes through the quadrangular space (a space bounded by the teres minor superiorly, the teres major inferiorly, the long head of the triceps medially, and the humerus laterally). The nerve divides into anterior and posterior branches once past the quadrangular space. The anterior branch passes between the humerus and the edge of the deltoid to then enter into the deltoid muscle and to innervate its middle and anterior thirds. The anterior branch also gives off a twig to supply cutaneous sensation to the skin overlying the inferolateral aspect of the deltoid muscle. The posterior branch supplies the smaller posterior third of the deltoid muscle as well as the teres minor muscle. The branch to the teres minor is given off just as the branch exits the quadrangular space. The posterior branch of the nerve then terminates as the upper lateral cutaneous nerve of the arm innervating the skin on the superolateral aspect of the shoulder. If the most proximal portion of the axillary nerve is being explored, i.e., that portion of the nerve proximal to the quadrangular space, then an anterior, infraclavicular brachial plexus approach is indicated. This is identical to that described for exposing the posterior cord to the radial nerve (see Chapter 5). If exposure of both the proximal and distal portion of the nerve is required, then the anterior approach may be combined with a posterior approach. If the two approaches are combined, a lateral decubitus, rather than a simple supine position, is required. For exposure of the axillary nerve in or beyond the quadrangular space or on both sides of the quadrangular space, the patient is placed in the lateral decubitus position.2 An axillary roll is placed under the contralateral (downside) arm. The free arm is placed on a draped and padded Mayo stand or in an airplane support or is freely draped in a stockinette. Elbows, knees, ankles, and wrists are padded to prevent any undue pressure on these areas. If grafting is anticipated, the lower extremities are prepped and draped to allow exposure of the sural nerves. The surgeon requires access to both the anterior chest wall and the posterior arm and scapula. For the posterior approach an incision is laid out similarly to that used to expose the radial nerve between the lateral and medial heads of the triceps (Fig. 3-1). The skin should be infiltrated with a vasoconstrictive agent such as lidocaine 1% with epinephrine in a 1:100,000 concentration and divided. The skin incision should expose the triceps muscle. The interval between the long and lateral head of the triceps can then be developed (Fig. 3-2). With blunt and sharp dissection the plane between the muscle is divided and the radial nerve is exposed at the depths of the split muscle (Fig. 3-3). The incision is extended until the deltoid muscle is seen to cross the field at a plane perpendicular to the triceps muscle, and the radial nerve can be traced proximally until the triangular interval. The triangular interval is signaled by the inferior border of the teres major muscle (Fig. 3-4). The axillary nerve is found exiting the quadrangular space at the superior border of the teres major muscle (Fig. 3-5). The quadrangular space is exposed with the teres minor muscle and its obliquely oriented fibers forming the superior boundary and the teres major the inferior boundary. The axillary nerve and the circumflex vessels are seen transmitted through this space (Fig. 3-6). The nerve may then be traced distally into the deltoid muscle as required.
AXILLARY NERVE
ANATOMY
POSITIONING AND SURGICAL EXPOSURE
< div class='tao-gold-member'>
Axillary Nerve
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree