15 Avoiding Complications
Basic Principles
Useful Strategies

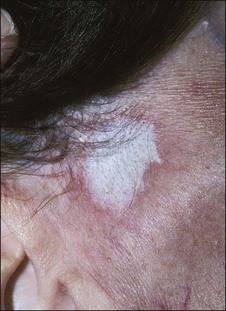
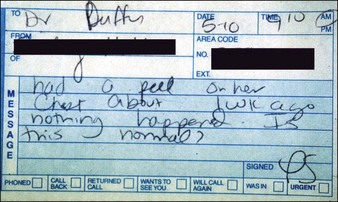
Figure 15.5 This patient has had an excellent result following a Baker’s peel without hyperpigmentation
See Boxes 15.1 and 15.2.
Educating Patients
• Discussing options
When discussing chemical peels with patients I arbitrarily divide them into three classes. Light peels, which are good for certain types of pigmentary disorder, textural abnormalities, and acne are described as ‘maintenance peels’ and do not require much downtime or carry much risk, but their results occur slowly (Fig. 15.7). Long term improvement is highly dependent on careful home programs which include the daily use of sunscreens and in many cases bleaching agents. Medium peels are described as capable of imparting a noticeable improvement in the patient’s appearance with the caveats of downtime while the patient is unpresentable, transient hyperpigmentation, and remote possibilities of more serious problems such as scarring. Deeper phenolic peels are described as more risky but absolutely necessary for deep wrinkles or severe photoaging. The possibility of serious complications, including hypopigmentation, scarring, systemic toxicity, and interaction with preexisting disease states or intraoperative medications, is carefully spelled out. I also discuss the medications we will be using or may need to use to carry out the procedure. These include local anesthetic with adrenaline, antibiotics, antiviral agents, and pain medications. It is also important to discuss the ‘no free lunch’ concept; that is, repeated applications of light peels ‘won’t make a dent in deep wrinkles’, but will often improve skin texture and dyspigmentation. Patients need to know that changes in skin color of either a transient or permanent nature are a major concern. As peels become deeper, the potential for permanent changes in skin color and lines of demarcation is greater (Fig. 15.8). Fair-skinned patients are told that there is a very high possibility of the skin being permanently lighter when deeper peels must be employed to efface deep rhytides. Very dark-skinned individuals are poor candidates for deep peels. Patients who tan well are told they might expect transient hyperpigmentation from any type of peel. Experience with curling irons and other forms of cutaneous trauma have often educated patients as to how their skin may respond to a peel.
The Psychology of Peels
Evaluating the Patient
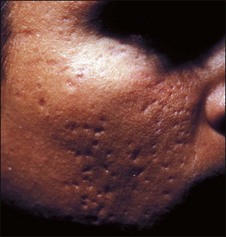
Patients exhibit their history on their skin (Fig. 15.9). Unlike other organs, this one is accessible. I ask them if they have been burned and look where they were burned. I ask them if they have had a brown spot after a burn or a light spot (Fig. 15.10). Look for surgical scars, ask about previous experience with burns (i.e., with curling irons) and whether the patient has had any procedures before. You frame your questions in the context of what effect something might have on the peel outcome. Do not forget to examine non-sun-exposed skin to see the patient’s true skin color.
• Personal habits/home regimens
Topical medications such as tretinoin (Retin-A), scrubs, cleansing granules, creams, and products bought at health food stores, as well as facial waxing, electrolysis, hair plucking, etc., can exert both preoperative and postoperative effects on peel outcomes (Fig. 15.11) Simple scrubbing to remove make-up immediately before a light peel can produce unexpectedly deep penetration of the agent. Sun exposure, certain types of medication, and certain skin types make a patient prone to specific types of complication.
• Sorting out patients
The most important evaluations have to do with patients who are going to need deep chemical peels. Patients with histories of hypertrophic scarring, dark-skinned patients, and patients with serious medical problems are not candidates for phenolic peels. Patients who do not use cosmetics (e.g., male patients) may be very poor candidates for deep chemical peels although they can certainly tolerate light and medium peels. I am particularly careful about employing periocular phenolic peels on patients who have had multiple blepharoplasties (Fig. 15.12) or who have undergone recent (less than 6 months) undermining plastic surgery or other types of resurfacing procedure. Heavy smokers are notoriously poor healers and are often poor candidates for deeper peels (Table 15.1).
Table 15.1 Factors in patient evaluation for phenol-based chemexfoliation
| General | General state of physical and mental health |
| Medications | |
| Pregnancy history | |
| History of herpes simplex | |
| Skin pigmentation classification evaluation | |
| History of hypertrophic scarring | |
| History of facial radiation or use of isotretinoin (Accutane) | |
| Realistic expectations | |
| Relative contraindications | Cardiac disease |
| Renal disease | |
| Hepatic disease | |
| Hormone replacement therapy | |
| Continued exposure to ultraviolet light | |
| History of radiation exposure or use of isotretinoin | |
| Contraindications | History of hypertrophic scarring or keloid formation |
| Fitzpatrick skin classification of IV–VI | |
| Recent facelift (deep chemical peeling in areas of recently undermined skin may result in vascular compromise and resultant scar formation) |
• Consultative ploys
I look for four things when I am evaluating a patient: