, Madan Ethunandan2 and Tian Ee Seah3
(1)
Poole Hospital NHS Foundation Trust, Poole, Dorset, UK
(2)
Department of Oral and Maxillofacial Surgery, University Hospital Southampton NHS Trust Southampton General Hospital, Southampton, UK
(3)
Orange Aesthetics and Oral Maxillofacial Surgery, Singapore, Singapore
Subunits and Anatomical Considerations
The pinna is a structure made up of a complex three-dimensional cartilaginous framework and draped by the skin on the lateral and medial aspects. The underlying elastic cartilage principally determines the shape of the ear. The skin on the anterior aspect is firmly adherent to the underlying cartilage and reveals the contours of the underlying cartilage, with minimal subcutaneous tissue. The skin of the posterior aspect is more loosely attached and contains more subcutaneous tissue.
The pinna lies between horizontal lines drawn from the superior orbital rim and the nasal spine. It protrudes from the scalp at an angle of 25–35°.
The skin on the lateral surface is thin and densely adherent to the underlying cartilage, whereas the posterior skin is thick and more mobile. The auricular cartilage is supple and can be easily deformed by wound tension and scar contracture. Scars can be camouflaged in the many undulations of the pinna. Local flap reconstruction often results in a decreased height of the pinna but when the shape and protrusion is maintained the discrepancy is surprisingly inconspicuous.
The goal of reconstruction is to try and preserve the shape, size and position of the pinna. Knowledge of the different parts of the pinna is essential for reconstruction (Fig. 9.1). When it comes to reconstructing auricular defects, it is more practical to analyse it in terms of (1) location, (2) extent and (3) composition of the defect.


Fig. 9.1
Landmarks of the Pinna
Special Considerations
Care when handling cartilage. Use 4.0/5.0 long-standing absorbable sutures, on a round bodied/tapercut needle to approximate cartilage. Take particular care to accurately approximate the helical rim, to prevent notching. Consider a pressure dressing to prevent the occurrence of a haematoma. Avoid clothing which needs to be removed over the head in the immediate postoperative period.
Concha (Cymba and Cavum) Defects
Healing by Secondary Intention
Indications
Partial-thickness defects (skin only/skin + cartilage)
Technique
The partial-thickness defect is left to heal by secondary intention. In case of skin-only defects, consideration can be given for perforating the underlying cartilage with a small punch biopsy core, to encourage granulation tissue ingress from the medial tissues. This can be useful, especially when perichondrium is lost.
Tips
A good wound care regimen is essential. The obvious disadvantage of this approach is the prolonged healing period and reliance on patient/carer co-operation. Distortion due to scarring can be minimised by careful case selection and restricting its use to small- and medium-sized defects.
Skin Grafts
Indications
Partial-thickness defects (skin only/skin + cartilage)
Technique
A suitable template is made of the defect, which is transferred to the donor site to harvest the graft. The graft is sutured to the defect, with additional “long” sutures that can be used for “tying” over the bolus. The graft can be “quilted” to the base, to decrease the risk of haematoma and dead space. A non-adherent dressing is laid over the sutured graft, over which a cotton wool ball/sponge soaked in proflavin or a suitable antibiotic ointment is placed. The tie-over bolus sutures are now used to hold the dressing in place. The sutures and pack are removed in 7–10 days time (See Fig. 9.5a–f).
Tips
For skin-only defects, consideration can be given for perforating the underlying cartilage with a small punch biopsy core, to encourage granulation tissue ingress from the medial tissues. This can be useful, especially when perichondrium is lost. Full-thickness grafts are preferred to split-skin grafts.
Revolving Door Flap
Indications
Medium and large skin + cartilage defects, posterior skin intact
Technique
A template is made to accurately reflect the defect and the dimensions marked out in the posterior auricular surface/mastoid skin, with the base centred along the auriculocephalic sulcus. The skin is circumferentially incised and undermined anteriorly and posteriorly, taking meticulous care to maintain a central subcutaneous pedicle, along the auriculocephalic sulcus. The flap is pulled through the defect, like a revolving door and sutured into the defect. The secondary defect is closed primarily by undermining the surrounding tissues (Fig. 9.2a–f).
Tips
The anterior margin of the flap in the posterior auricular surface is marked out to overlap the underlying cartilage defect. The pinna will be “pinned” back, when the secondary defect is closed. This can interfere with the fit of an existing hearing aid and would have to be discussed with the patient.
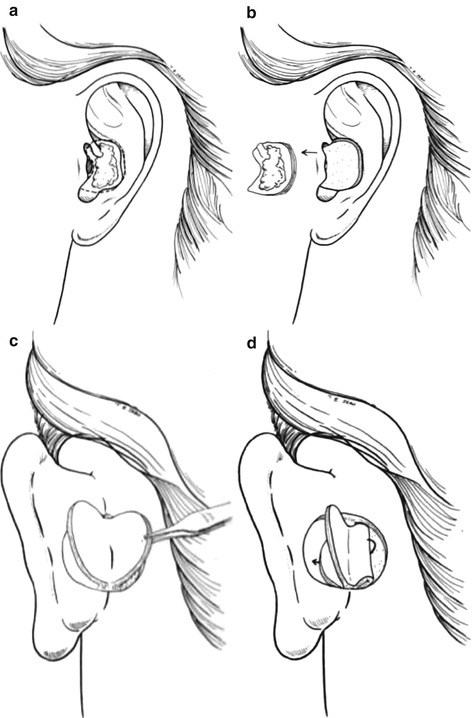
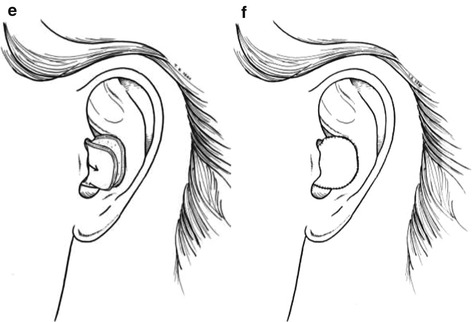
Fig. 9.2
Revolving door flap
Postauricular Artery Island Flap
Indications
Skin + cartilage defects, posterior skin intact
Technique
An accurate template is made of the defect and the dimensions marked on the mastoid skin. The flap is incised laterally, superiorly and medially down to the periosteum, but only through the skin inferiorly, to maintain the vascular pedicle. Inferiorly the skin is raised in the subcutaneous plane and the island flap elevated deep to the vascular pedicle (postauricular artery/postauricular muscle), on the surface of the periosteum. The required mobility is obtained by undermining the flap inferiorly around the pedicle. A tunnel is created from the anterior margin of the flap into the defect. The flap is mobilised into the defect and sutured into place. The secondary defect is closed primarily by undermining the surrounding tissues (Fig. 9.3a–e).
Tips
Care should be taken to avoid damage to the pedicle during dissection and transfer. The tunnel should be of an adequate dimension to avoid compression of the pedicle. The pinna will “not” be pinned back with this procedure and can be an alternative to the revolving door flap, if this an important consideration.
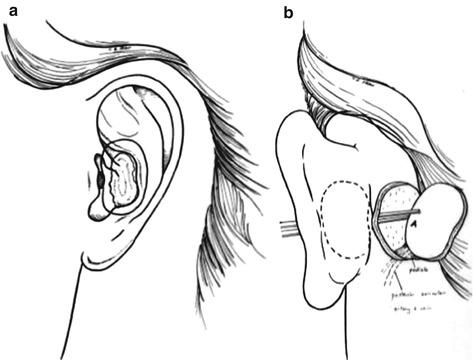
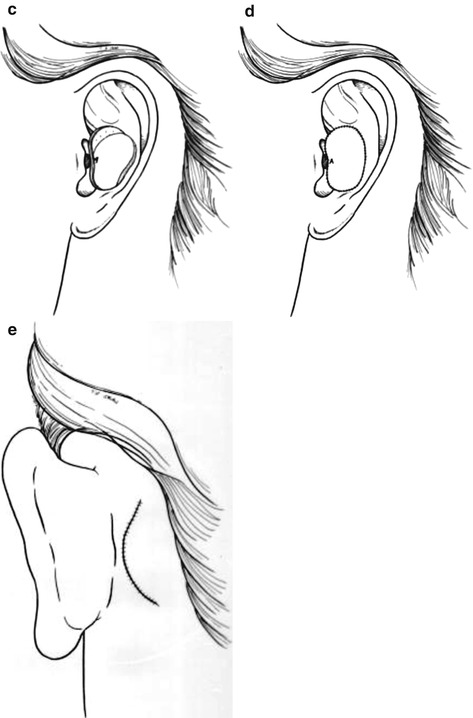
Fig. 9.3
Post auricular artery island flap
Postauricular Transposition Flap
Indications
Skin + cartilage defect, posterior skin intact
Technique
A template is made to accurately reflect the defect and the dimensions marked out in the posterior auricular/mastoid skin. The flap can be raised on a superiorly or inferiorly based pedicle, consisting of the skin, subcutaneous tissue and postauricular muscle. The margins of the flap are incised down to periosteum and the flap raised in the supra-periosteal plane. The flap is tunnelled anteriorly through to the conchal defect and sutured into place. The section of the flap passing through the tunnel can be de-epithelialised, in case of a one-stage reconstruction. Alternatively, the flap pedicle is left intact and can be divided after 3 weeks as a two-stage procedure and inset into the defect. The secondary defect can be closed primarily by undermining the surrounding tissues (Fig. 9.4a–h).
Tips
The tunnel should be of an adequate dimension to avoid compression of the pedicle. The pinna will be “pinned” back, when the secondary defect is closed. This can interfere with the fit of an existing hearing aid and would have to be discussed with the patient.
Fig. 9.4
Post auricular artery transposition flap
Antihelix Defects
Healing by Secondary Intention
Indications
Partial-thickness defects (skin only/skin + cartilage)









