CHAPTER 8 Atopic Eruption of Pregnancy
Introduction
Atopic eruption of pregnancy (AEP) has recently been introduced as a new disease complex among the specific dermatoses of pregnancy. It encompasses eczema in pregnancy, prurigo of pregnancy, and pruritic folliculitis in pregnancy, as a large retrospective study on more than 500 pregnant patients with pruritic skin diseases has demonstrated significant overlap between these three conditions1. AEP is by far the commonest pregnancy dermatosis, accounting for approximately 50% of pruritic rashes in pregnancy. Its clinical spectrum includes eczematous and papular lesions in patients with a personal and/or family history of atopy. Although AEP manifests throughout pregnancy, affecting all three trimesters, it usually presents much earlier than the other specific dermatoses of pregnancy (75% onset before the third trimester)1. AEP usually responds quickly to therapy and fetal prognosis is not endangered.
Historical background
Atopic eczema is a chronic, relapsing, pruritic dermatitis, affecting 1–5% of the general population. The prevalence of this condition appears to be increasing, possibly because of environmental changes.2–4 Several previous studies have shown an exacerbation of eczema during pregnancy5. Kemmett and Tidman5 noted that 50 of 150 atopic women reported a premenstrual exacerbation of the symptoms of atopic dermatitis. Similarly, in 50 women with previous pregnancies, pregnancy had had an adverse effect in 52% of cases, usually in the first and second trimesters5. In a recent prospective study of 200 women with rashes in pregnancy, eczema was found to be the commonest pregnancy dermatosis, accounting for 36% of the total number of cases6. So far, these important findings had not been acknowledged by any of the classifications on pregnancy dermatoses. Since the very first reports, however, there had been doubt that prurigo of pregnancy and pruritic folliculitis of pregnancy represented distinct entities. Holmes and Black7 suggested that prurigo of pregnancy may simply result from pruritus in atopic women rather than being a distinct entity.
Going back to the first description of prurigo of pregnancy, by Besnier et al. in 19048, it must be acknowledged that “prurigo” at that time was the term applied to describe the condition known as atopic dermatitis nowadays. A comprehensive retrospective study recently evaluated anamnestic, clinical, and histo/immunopathologic data in a series of more than 500 pregnant patients with pruritic skin changes. Significant overlap, both clinically and histopathologically, was demonstrated among patients with eczema, prurigo, and pruritic folliculitis of pregnancy (see Chapter 9)1. Based on these observations, the term “atopic eruption of pregnancy” has been introduced, resulting in a simplified classification of pregnancy dermatoses, as outlined in Chapter 4.
Etiology
Pregnancy is known as an immunologic state where a natural homeostasis exists between antigenically different tissues. To prevent fetal rejection, normal pregnancy is characterized by a lack of strong maternal cell-mediated immune function and TH1 cytokine production (e.g., interleukin (IL)-12, interferon-gamma) and a dominant humoral immune response and TH2 cytokine production (e.g., IL-4, IL-10)9. These distinct changes in TH1/TH2 cytokine balance are considered responsible for the remission in predominant TH1-driven autoimmune diseases during pregnancy and their characteristic deterioration in the postpartum period, as observed in rheumatoid arthritis or multiple sclerosis, compared to a flare in pregnancy of mainly TH2-driven autoimmune diseases, such as systemic lupus erythematosus10. As atopic dermatitis overall is considered to be a TH2-dominant disease, which accounts especially for acute lesions,11,12 it has been postulated that the TH2 shift associated with pregnancy may favor the exacerbation of atopic dermatitis during pregnancy as well as the manifestation of AEP. Howarth13 postulated that the persistence of this placental TH2 drive may be a major factor in the increasing prevalence of allergic disease over the past 30–40 years.
Clinical and diagnostic features
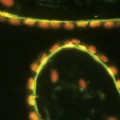
In 20% of cases, there is an exacerbation of pre-existing atopic dermatitis with the typical clinical appearance. Acute lesions, such as pruritic, erythematous papules and vesicles, or extensive weeping areas covered with serous exudates may be present as well as subacute and chronic features, including excoriated papules and plaques, scaling, and lichenification (Figures 8.1–8.3).
Eighty percent of patients, however, experience atopic skin manifestations for the first time ever during pregnancy, or after a long remission (i.e., childhood eczema). Most patients will give a positive personal history of atopy or a family history of asthma, eczema, or hayfever in a first-degree relative. Morphologically, two-thirds of patients display patchy eczematous changes (E-type AEP) (Figures 8.4–8.7), whereas one-third present with papular lesions (P-type AEP) (Figures 8.8–8.12)1. The latter occur as prurigo lesions or disseminated, small erythematous papules. Typical atopic sites such as face, neck, anterior chest, and flexural surfaces of extremities are often involved. Overall severe dryness of the skin and frequent atopic “minor features” according to Hanifin and Rajka14 are common findings. Histopathology is nonspecific and varies with clinical presentation; direct and indirect immunofluorescence are negative. Total serum immunoglobulin (Ig) E levels are elevated in 20–70% of cases.