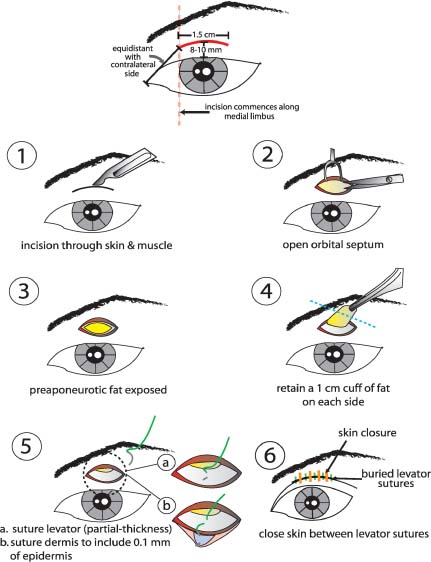
8 Creation of a supratarsal crease for the Asian patient may be achieved through a variety of surgical strategies. In fact, the number of permutations of surgical technique that exists closely matches the number of surgeons who practice double-eyelid surgery, as every surgeon performs a slightly different modification to suit his or her own preference. Perhaps the simplest categorization that can offer the reader comprehension of the myriad techniques that exist for double-eyelid surgery is to divide the techniques into three major types: full-incision, partial-incision, and suture technique.1 This simplified classification is not meant to imply that all techniques fall neatly into these groupings. For instance, some surgeons prefer to perform a near full incision but stop short laterally. Other practitioners advocate a suture technique via a limited, partial-incision approach.2,3 Alternatively, a full incision can be undertaken, and only part of the levator length fixated to the dermis, as performed in the partial-incision method. All of these many techniques have been proven with considerable clinical experience and are viable in the right surgical hands. The full-incision technique has already been thoroughly covered in Part I of this book and will not be reiterated herein.4 This chapter is devoted to a detailed review of the two major alternative strategies for double-eyelid creation: the partial-incision and the suture technique. After reviewing numerous permutations of these two principal methods, the author has selected two techniques that celebrate simplicity and elegance and that are established upon a substantial clinical experience. The author relies principally on the partial-incision method to undertake most of his surgical endeavors and selects the full-incision technique only when redundant skin must be removed, such as in the older individual seeking double-eyelid creation. The suture technique is reserved for patients who have relatively little adipose tissue (that would otherwise obstruct a favorable dermal-levator adhesion) and who express interest in this surgical modality. The partial-incision technique developed by Young Kyoon Kim offers an ideal balance between the full-incision and the suture methods.5 The limited incision that spans only about one-third of the total eyelid length offers a rapid and reliable method for double-eyelid creation and limits postoperative edema and risk of scarring (Fig. 8-1). Unlike the aging eyelid, the medial fat compartment is rarely addressed in double-eyelid creation. Even if a full incision is undertaken, only the central fat compartment is resected, as removal of the medial fat may predispose toward scarring and is simply not necessary. Accordingly, the abbreviated incision involved with the partial incision affords easy access to the central fat compartment to reduce the “puffy” eyelid appearance characteristic of the Asian upper eyelid. Furthermore, an incision that extends toward the medial canthus increases the risk of cutaneous scarring and webbing, as the medial aspect of the Asian eyelid has a natural propensity for cicatricial formation. Therefore, the partial-incision technique permits removal of the only fat compartment that needs to be addressed and access to the levator aponeurosis for placement of fixation sutures that will yield a fold that extends across the entire eyelid despite the relatively short length of suture fixation. Figure 8-1 This schematic illustration demonstrates the stepwise approach to the partial-incision double-eyelid technique. The incision measures ~1.5 cm in diameter and begins medially at the medial limbus to span one-third of the eyelid distance. Symmetry should be well established with Castroviejo calipers before commencing surgery. Step 1: After a precise amount of local anesthesia is infiltrated into each incision (0.3 cc per side), the incision is made through the skin and muscle with a no.15 Bard-Parker blade. Hemostasis is achieved with bipolar cautery. Step 2: The orbital septum is incised and excised until the underlying postseptal adipose tissue is freely released. Step 3: With the preaponeurotic (postseptal) fat exposed, the contralateral eyelid should be approached in the same fashion until the fat is similarly encountered. Step 4: A 1-cm cuff of fat should be retained on each side to avoid a hollow-eye appearance. Step 5: The levator (a) to dermis (b) should be fixated passing the suture in a partial thickness fashion through the levator from superiorly to inferiorly then through the dermis up to include 0.1 to 0.2 mm of the epidermal edge from superiorly to inferiorly. The suture is tied down with one knot and the patient is asked to open his or her eyes to confirm adequate fixation and height of the eyelid crease as well as observation of slight eyelash eversion. The contralateral eyelid is undertaken in the same manner, and symmetry is confirmed. A total of seven levator-dermal fixation sutures are placed in each eyelid. Step 6: The skin is then closed with interrupted sutures between the buried levator sutures. The partial-incision method offers the distinct advantage over the suture method in that the central fat compartment can be readily addressed and the longevity of crease fixation may be superior as well (although this point may be debated). As the length of fixation is shorter than with the full-incision technique, the chance of crease loss is potentially higher, but correction of this problem is simpler than with the full-incision technique. The full incision also permits modulation of the medial-canthal region by extending the incision toward the epicanthus if an epicanthoplasty is required. Nevertheless, an epicanthoplasty can still be undertaken concurrently with the partial-incision method using a separate, abbreviated incision along the epicanthus. The full-incision method also permits creation of a fold that follows a more precisely prescribed contour (e.g., an inside vs. outside fold). With the full-incision method, the outer shape of the eyelid can also be more effectively adjusted, for example, shaping an oval or round eyelid appearance.* In addition, excessive eyelid skin or muscle cannot be readily addressed with the partial-incision method. Accordingly, the partial-incision technique is ideally suited for younger patients who are in their teenage years and 20s. To compensate for the patient with excessive skin redundancy, the incision height may need to be adjusted superiorly to achieve the desired crease height. (The reader is referred to the following section on surgical technique for details.) Depending on the amount of skin redundancy and the height of the incision, an inside or outside fold will arise with the partial-incision method: greater skin redundancy and a lower crease height will predispose toward an inside-fold configuration, whereas less skin redundancy and a higher crease height will most likely yield an outside fold. If the patient does not express any significant desire to have one type of fold or the other, the partial-incision method may be undertaken for its technical ease, rapidity, and faster postoperative recovery. If the patient desires a precise shape and contour of the fold, then a full-incision method may be warranted. If revision surgery is required, the partial-incision method facilitates a faster, less labor-intensive undertaking compared with one that follows the full-incision method. As part of this spectrum, the suture technique is associated with the simplest and fastest revision surgery. The patient should receive a detailed preoperative consultation that enumerates all of the potential advantages and disadvantages of each of the surgical methods so that an educated and informed judgment can be rendered as to the optimal technique for that individual.
Asian Upper Blepharoplasty: The Partial-Incision and Suture Techniques
♦ General and Anatomic Considerations
♦ The Partial-Incision Technique
Method of Young Kyoon Kim Preoperative Remarks
Surgical Technique
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree