CHAPTER 33 Arthrodesis of the Hallux Metatarsophalangeal and Interphalangeal Joints
ARTHRODESIS OF THE HALLUX METATARSOPHALANGEAL JOINT
Approach to Arthrodesis
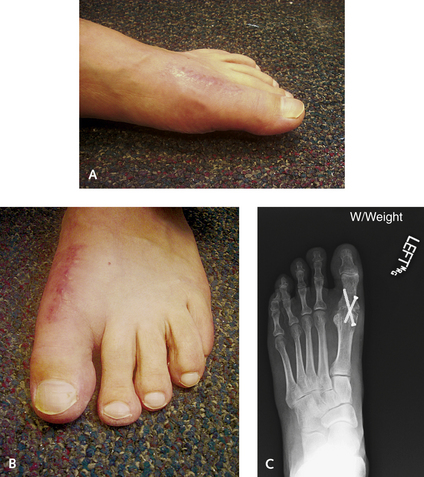
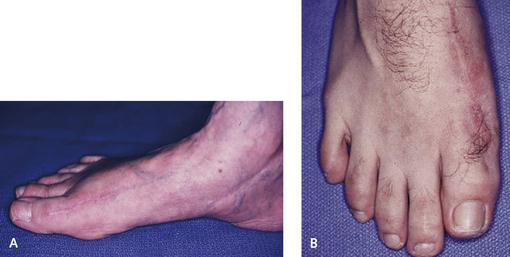
Arthrodesis of the hallux metatarsophalangeal (MP) joint is indicated for correction of deformity, to treat arthritis, and to address neuromuscular imbalance of the MP joint (with or without deformity). As a generalization, this is an operation that is technically easy to perform, with a predictable outcome, provided that the hallux is well positioned. Although the focus of the procedure is on the MP joint, the presence of interphalangeal (IP) joint instability, hyperextension, or arthritis may preclude a successful outcome of the arthrodesis. The key to this operation is in the correct positioning of the arthrodesis: The hallux must be slightly supinated into a neutral position, in slight dorsiflexion with respect to the correct position of the floor, and in slight valgus. Some of these parameters will need to be modified depending on patient characteristics and preferences (e.g., the running athlete, the patient who desires to wear slightly higher-heeled shoes) (Figures 33-1 and 33-2). With arthrodesis performed for correction of severe hallux valgus, a straight toe is not tolerated, and the hallux should be fused in 5 to 10 degrees of valgus (Figure 33-3).
Alignment of Arthrodesis
Therefore the decision regarding how much dorsiflexion to incorporate into the fusion has to be made after consideration of various factors including the presence of any preexisting hyperextension and instability of the IP joint and the patient’s types and level of activity, sports interests, and shoe wear needs (Figure 33-4). Fusion of the hallux MP joint at an angle is preferable to the position of the floor rather than the metatarsal. The metatarsal declination varies considerably, and the more predictable position would be with reference to the floor. In the setting of a cavus foot or a steep plantar flexed first metatarsal, however, arthrodesis of the hallux MP joint will result in pain under the first metatarsal head and sesamoiditis. If MP joint fusion is the only possible treatment option in the setting of a fixed forefoot equinus or plantar flexed first ray, a dorsal wedge osteotomy of the first metatarsal may have to be performed before proceeding with the arthrodesis. The converse applies in a patient with severe elevatus of the first metatarsal. Here, position of the fusion relative to the metatarsal may be in neutral alignment, but the hallux remains elevated relative to the floor. Not much, if any, dorsiflexion can be incorporated in the hallux MP joint in patients with metatarsus primus elevatus.
The alignment of the hallux in the coronal plane must be accurate. If the hallux is overpronated, pain will be present at both the medial aspect of the IP joint and the medial margin of the nail, with consequent ingrowth of the toenail (Figure 33-5). Pronation of the hallux MP joint fusion will lead to marked fixed deformity of the IP joint in flexion and valgus, which is very difficult to correct. If indeed this deformity develops, the MP fusion should be revised to prevent fixed changes with arthritis in the IP joint. Oversupination leads to pain on the medial or lateral nail fold, and an ingrown toenail can result as well. The best way to check alignment of the hallux is to look at the way the hallux nail lines up with the adjacent toenails.
Sesamoid Issues
Occasionally patients experience sesamoiditis after arthrodesis of the hallux MP joint. If present, this condition usually is the result of soft tissue atrophy under a plantar flexed first metatarsal, rather than painful arthritis between the sesamoid and the first metatarsal head. If the latter occurs, it can be secondary to a hypertrophy of the sesamoid. It cannot always be anticipated, and a sesamoidectomy may need to be performed at a later date after the arthrodesis. If the patient has sesamoid pain (from pressure) preoperatively, however, the sesamoid can be resected in conjunction with the arthrodesis of the hallux MP joint. It is possible to resect the sesamoid(s) through the dorsal incision. If such resection is anticipated, a medial approach to the MP arthrodesis can be used, making the sesamoidectomy easier to perform. If symptoms of pain under the metatarsal head occur after arthrodesis, removal of the sesamoid is very easy from a direct medial approach to the MP joint.
Bone Grafting
Bone graft is not used for the standard MP fusion and is necessary only when either shortening of the hallux, osteolysis, or cystic defects are present. To correct a very short hallux or one for which graft is clearly required, the decision is between fusing the hallux in situ with cancellous bone graft and using a bone block graft to lengthen the hallux. Clearly, if severe shortening of the hallux is present with transfer metatarsalgia, then an arthrodesis with a bone block graft would be ideal. Even with minor bone loss, although an arthrodesis is technically feasible, some further shortening of the hallux always occurs as a result of preparation of the joint surfaces; from a functional as well as a cosmetic standpoint, even minimal shortening is undesirable (Figures 33-6 and 33-7). If an in situ arthrodesis is performed when metatarsalgia is present, then either shortening osteotomies of the lesser metatarsals or metatarsal head resection should be considered. With the current custom plates designed specifically for use with a lengthening arthrodesis of the MP joint, as well as the use of orthobiologic agents, my preference usually is to lengthen the MP joint with a structural bone graft (Figure 33-8).
Approach and Joint Preparation
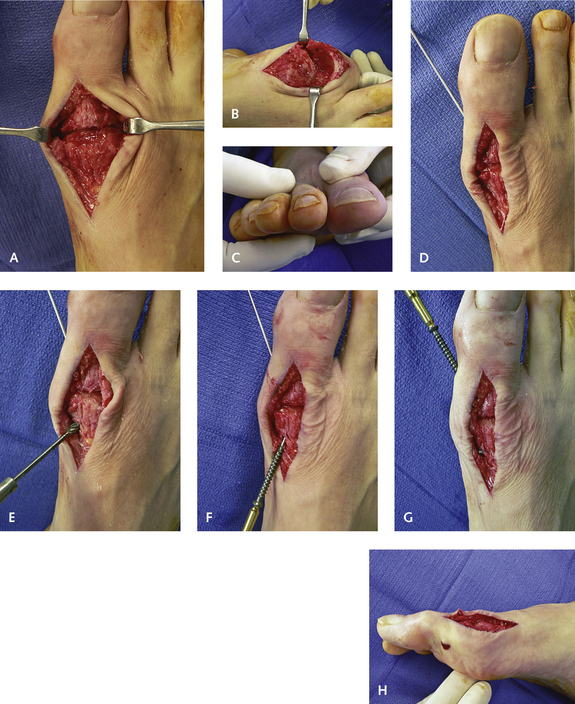
The technique for arthrodesis of the MP joint with standard exposure and crossed cannulated screw fixation is demonstrated in Figure 33-9. The incision is made medial to the extensor hallucis longus (EHL) tendon, over a length of 4 cm, with a small cuff of extensor retinaculum left for later closure. The extensor tendon is retracted laterally, and using subperiosteal dissection, the entire articulation is exposed. Forcibly plantar flexing the proximal phalanx is helpful; plantar flexion facilitates dissection of the periosteum off both sides of the joint. With further plantar flexion of the hallux, the undersurface of the proximal phalanx, including the attachment of the volar plate, is easily dissected. Stripping the attachment of the sesamoids is unnecessary because they retract once the volar plate is released.
Fixation
For a straightforward arthrodesis with good bone support, I typically use cannulated 4.0-mm screws for fixation. Of note, use of partially threaded screws is not necessary, because broad cancellous bone surfaces are present, and the fusion requires rigidity and stability as much as compression. Nonetheless, if the bone quality is good, I currently use partially threaded screws. With the hallux in the reduced position, guide pins are introduced to cross the articular surface. The first guide pin is introduced from the plantar medial aspect of the undersurface of the metatarsal neck just proximal to the metatarsal head. This pin is aimed distally and passed out of the metatarsal head and into the lateral base of the proximal phalanx. It is useful to make a small pilot burr hole as a countersink maneuver before inserting the guide pin. The second guide pin is introduced from distal to proximal from the medial aspect of the base of the proximal phalanx across the metatarsal head and exits slightly dorsally and laterally. If the bone on the base of the phalanx or medial head is inadequate (as, for example, after bunionectomy), one of the screws is introduced from the dorsal neck of the metatarsal head distally into the phalanx.
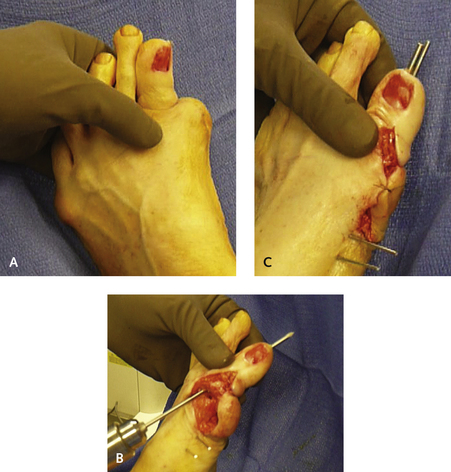
Sometimes the standard screw fixation is not sufficient because of the plane of the metatarsal head or the proximal phalanx. This problem may arise, for example, after failed bunionectomy, when a medial eminence is not present and less of an anchor point is available for the head of the screw. If bone loss is a factor or if the contour of the metatarsal head does not facilitate internal fixation, other means of fixation must be used instead of screws. Alternatives include a dorsal plate, multiple threaded small K-wires, and large threaded Steinmann pins (Figure 33-10). Clearly, crossing the hallux IP joint is not desirable but is necessary with use of the larger threaded pins. Sometimes, however, the bone loss is so severe that the MP joint has to be anchored with the distal phalanx for support. An anchoring method that I have found to be very stable is to use one crossed oblique 4.0-mm partially threaded screw supplemented by a custom dorsal MP fusion plate (Orthohelix, Akron, Ohio).
Correction of Deformity Associated With Bone Loss
In cases with severe bone resorption or bone loss, an in situ arthrodesis is not sufficient, and structural support with an interposition graft must be considered. With the use of custom-designed plates and added orthobiologic agents, structural grafting has now become a relatively easy procedure to perform. For selected patients, such as those with severe bone loss and erosive synovitis associated with failed implant arthroplasty, the surgery can be staged. For these patients, I remove the implant, resect the fibrinous debris, lengthen the EHL tendon, and fill the defect in the phalanx and metatarsal head with cancellous bone graft. After 6 months, once the graft has incorporated, the second-stage structural graft–fusion procedure is performed. Some patients, however, are reasonably comfortable after the first stage of the surgery, so the second stage with arthrodesis is not performed. Although the hallux remains short and weak, the pain from the inflammatory synovitis dissipates, and function is acceptable. Another alternative is to stage surgery by removing all debris, hardware, and necrotic bone, in particular when the possibility of infection is a concern. A good example is presented in Figure 33-11. In the case illustrated, the patient underwent multiple unsuccessful surgical attempts at an MP arthrodesis, resulting in a nonunion, as well as a questionable nonunion of the tarsometatarsal joint and possible chronic infection. The hardware was removed, and after culture samples were obtained, antibiotic-impregnated cement was inserted as a spacer to maintain bone length; the second-stage surgery was performed 6 weeks later with a bone block lengthening arthrodesis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree