SURGICAL APPROACHES TO THE ORBIT
John L. Wobig and Roger A. Dailey
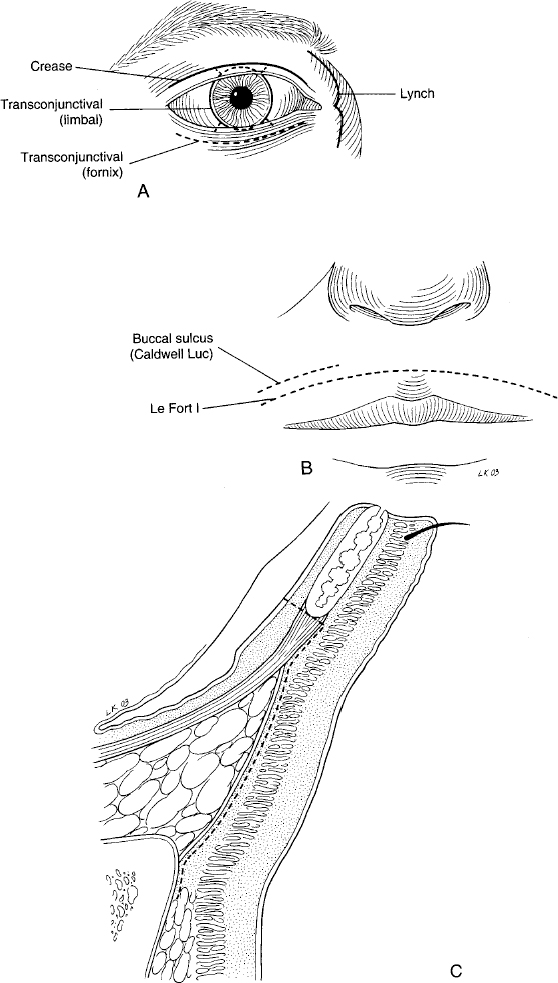
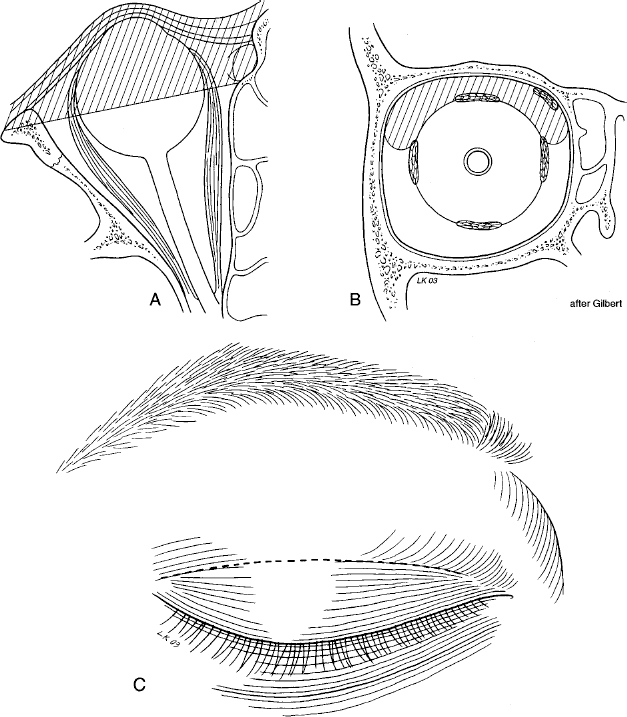
The orbit is subject to numerous maladies; many of which are best managed by surgical intervention. The most reasonable approach to obtain access to these varied problems is largely determined by the nature, location, and extent of the problem. Fig. 16-1A,B,C demonstrates the various incisions used to access the orbit.
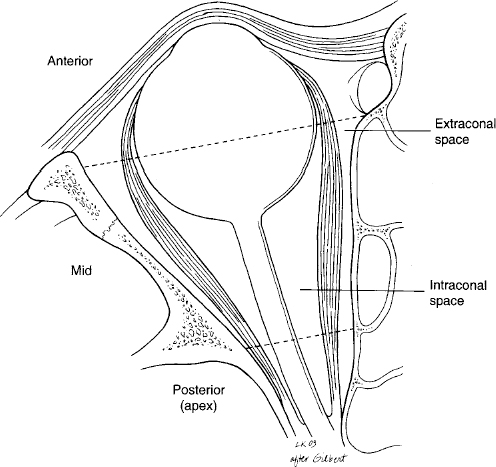
The most anterior portions of the orbit not involving bone can be accessed through both skin and conjunctival incisions, utilizing local infiltrative anesthesia with or without intravenous sedation (Fig. 16-2). Access to the tissues posterior to the equator of the globe, but not the apex, can occasionally be gained this way but often will require general anesthesia and a more extensive orbitotomy or combination of procedures. For apical access and bone manipulation, the patients usually do better with general anesthetic.
A combination of blunt and sharp tissue manipulation is required for dissection in the orbit. Because of the large number of important structures in such a small area, blunt dissection is favored until the anatomy is very clear. One of the biggest challenges of operating in the orbit is the seemingly ever present, ever visually obstructive orbital fat. Wide ribbon retractors are essential to retract this fat for good visualization. A skilled assistant can be extremely helpful in more extensive, deep, complicated orbital cases. A good headlight for the surgeon for deeper cases is essential.
In addition to the standard soft-tissue, ophthalmic, facial plastic surgery instruments, the operating room staff will need to have available a moderate-sized, self-retaining orbital retractor along with a drill with a 1.5 mm bit and dental burr. If bone is to be removed immediately adjacent to delicate soft tissues such as the dura or the optic nerve, a diamond burr should be used. A sagittal saw, Lempert style bone rongeurs, ribbon retractors, toothed bayonet forceps, straight and curved bayonet neurosurgical scissors, small periosteal elevator, and blunt hook should be available.
Hemostasis is critical to visualization during surgery and prevention of vision loss via retrobulbar hemorrhage postoperatively. A monopolar cautery (Valleylab, Boulder, CO) can be used to cut or cauterize subcutaneous tissue and the tissue generally connected to bone. In the soft tissues of the orbit however, bipolar cautery is suggested to prevent collateral damage to important structures. Neurosurgical cottonoid sponges are not only useful to aid in visualization during surgery but soaked in thrombin with or without Gelfoam (Pharmacia & Upjohn, Kalamazoo, MI) are extremely useful for hemostasis. The surgeon can continue to use suction (on the cottonoid sponges) without occluding the tip or sucking up the Gelfoam if it has been placed. For most cases surgical drains are not needed. In cases where some continued bleeding or fluid collection is anticipated, a drain may be placed at the time of closure and brought out through a separate stab incision and connected to passive bulb suction. The drain can usually be pulled on the first postoperative day.
UPPER EYELID CREASE INCISION
For pathology located in the superior orbit that is anterior and above the levator, this approach works nicely and the resultant scar is well hidden in the normal crease (Fig. 16-3A,B,C). The lacrimal gland is easily accessed for biopsy such as in cases of lymphoma or benign dacryoadenitis. If a benign mixed tumor of the gland is anticipated, a lateral orbitotomy approach is probably better to allow removal of the entire tumor and surrounding tissues. Additional types of cases where a crease incision would be useful are biopsy for amyloidosis, draining a spontaneous subperiosteal hemorrhage or abscess, or removal of a foreign body. Excellent exposure of the superior oblique tendon and trochlea can be obtained with this approach, and it is the preferred route to identify and cannulate the superior ophthalmic vein for embolization of arteriovenous fistulas recalcitrant to the standard approach from the femoral artery.
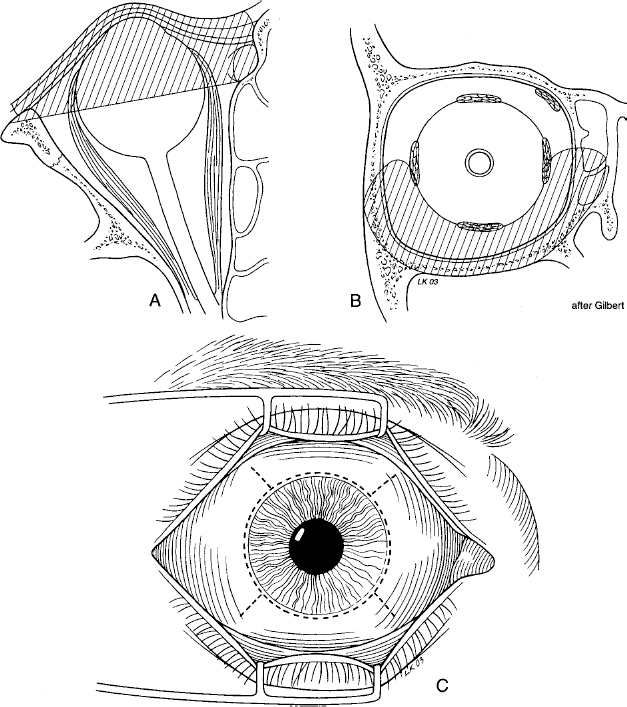
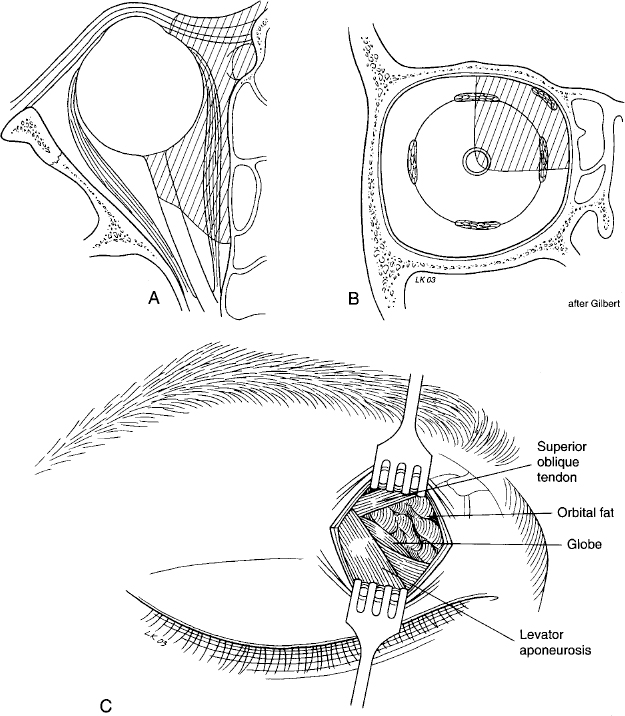
Pelton and Patel describe a superomedial lid crease approach to the medial intraconal space for optic nerve sheath fenestration and removal of tumors in this area (Fig. 16-4A,B,C). An upper eyelid splitting procedure has also been advocated for surgery in this area but is potentially more disfiguring. Therefore, it would seem that for access to this area, the medial lid crease approach has several advantages over the medial transconjunctival, lid splitting, and lateral orbital approaches described following here. These include ease of dissection, incision-to-nerve distance, and the angle of approach to the optic nerve.
SURGICAL TECHNIQUE
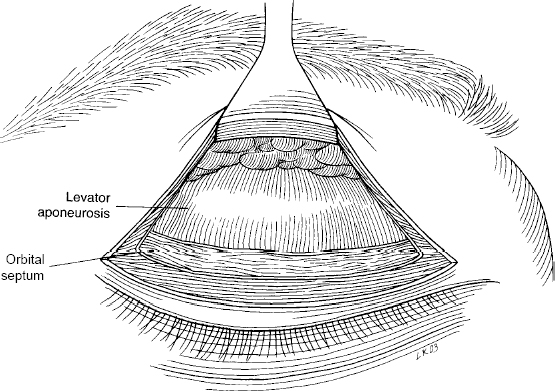
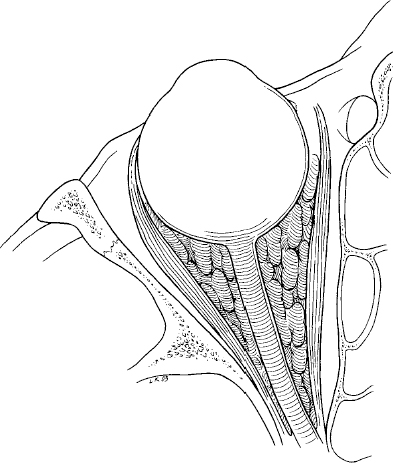
For standard superior crease orbitotomy, the surgical incision can be made anywhere in the upper eyelid crease. The orbicularis muscle is then divided or a small portion resected the length of the incision. Once the orbital septum is identified, it is incised the entire length horizontally in the incision allowing access to the anterior orbit superior to the levator aponeurosis (Fig. 16-5). The levator and globe can be retracted inferiorly. Care must be taken to avoid injury to the superior oblique tendon and trochlea medially. Dissection proceeds in a blunt fashion. The lacrimal gland is found temporally in its fossa, lateral to the lateral horn of the levator aponeurosis. It has a generous arterial supply. Access to the subperiorbital space is easily gained by sharp dissection superiorly.
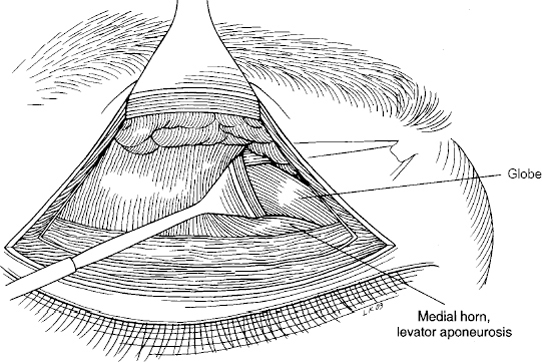
The medial intraconal space is entered medial to the medial horn of the levator aponeurosis, which is retracted laterally (Fig. 16-6). The superior oblique tendon and orbital fat are retracted superiorly and the globe inferiorly. Blunt dissection continues in a lateral and inferior direction until the tumor or the optic nerve is encountered. The superior ophthalmic vein can be gently retracted superiorly and care is taken to avoid the vortex veins. The posterior ciliary vessels near the optic nerve are avoided but serve as a good landmark of nerve location.
Approximation of the skin is typically all that is required for closure of this type of wound. A drain is rarely required.
TRANSCONJUNCTIVAL APPROACH
The anterior medial, inferior, and lateral quadrants of the orbit can be accessed through a conjunctival incision (Fig. 16-7A,B,C). The traditional incisions are the medial peritomy, lateral peritomy, superior transconjunctival in the superior fornix, and transconjunctival approach in the lower fornix. All four quadrants of the intraconal mid-orbit can also be accessed this way with release of the corresponding rectus muscle from the globe. The muscle is reattached to the globe at closure. The relatively small surgical field limits the visualization and removal of tumors via this approach. Practically, this approach is good for biopsies, access to extraocular muscles, and removal of anterior tumors and those located in the anterior intraconal space. Medial optic nerve sheath decompressions can be performed in this fashion. They should not be used to gain access to the orbital bones.
For discussion purposes, the medial peritomy transconjunctival approach to the medial intraconal space will be discussed and illustrated as representative of the transconjunctival technique (Fig. 16-8). This is commonly used for optic nerve sheath fenestration and removal of tumors in this area. As was mentioned earlier, this location can also be reached through a medial lid crease or lid splitting incision.
SURGICAL TECHNIQUE
With the patient in a supine position on the operating table under monitored anesthesia care or general anesthesia, the conjunctival peritomy is made medially with superonasal and inferonasal relaxing incisions (Fig. 16-9). The superior and inferior nasal quadrants are then opened with a spreading motion using blunt Stevens tenotomy scissors. The medial rectus muscle can be disinserted from the globe for access to the intraconal space at this point if necessary. The globe is then retracted laterally with a Dailey globe retractor (Bausch & Lomb, Rochester, New York), and the medial rectus muscle and orbital fat are retracted medially with a ribbon retractor (Fig. 16-10). Blunt and sharp dissections are utilized to find the optic nerve for fenestration. In the case of a cavernous hemangioma in this region, a cryoprobe can be used to attach to the tumor and provide gentle traction to facilitate removal (Fig. 16-11). The medial rectus muscle is then reattached to the globe, utilizing double armed 5-0 Vicryl (910 polyglactin) suture.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree