Lasers in surgery and medicine have evolved into a specialized area with increasing use and innovative techniques requiring anesthesia providers to be familiar with the historical, technical, and procedural aspects of laser applications.
Lasers applications in surgery include a variety of procedures with various laser types and specific anesthetic considerations.
Currently, anesthesia providers commonly encounter use of lasers in many procedures including airway surgery, cutaneous and cosmetic surgeries and various urologic procedures.
Development of an anesthetic plan that is safe and satisfactory to the surgeon and patient necessitates knowledge of the procedure and patient characteristics.
Use of lasers for procedures in pediatric patients include dental procedures, dermatologic and laryngeal surgery each having special anesthetic considerations.
In obstetrics and gynecology, monitored anesthesia care is used for procedures using lasers ranging from laser conization to in utero coagulation of placental vascular anastomosis for twin-to-twin transfusion syndrome.
With the use of lasers in the operating becoming more common in recent years, awareness and adherence against health hazards to both the patient and personnel is essential.
Laser safety includes vigilance on the part of the anesthesia provider to prevent laser induced fires, avoid eye injury and burns, as well as, prevent electrical hazards.
Introduction
Laser applications for surgery are widespread and include excisions of dermatologic lesions, treatment of laryngeal lesions, pediatric dentistry and treatment of prostatic hypertrophy. Procedures involving lasers and the airway represent a special challenge to the anesthesia provider including risk of airway fire, aspiration, injury, and inadequate ventilation and oxygenation. Use of laser in cosmetic and cutaneous procedures is generally well tolerated with monitored anesthesia care supplemented with topical or local anesthesia. Laser use in prosthetic reduction surgery is common and often patients are elderly presenting with multiple co-morbidities influencing choice of anesthetic technique. Anesthesia for procedures involving laser use in specialized patient populations such as pediatrics and obstetrics requires the anesthesia provider to be familiar with the procedure and special needs of the patient. As laser technology continues to evolve in the fields of medicine, surgery, and dentistry, benefits to the patient as it relates to anesthesia are apparent in some areas and require further study in others. Laser safety programs are required nationally in all hospitals and office based surgical facilities using lasers. |
History
The medical application vand uses of the laser have increased greatly over the past 40 years. Currently lasers are used for cauterization, tumor ablation, bloodless surgery and generally where destruction of a pathologic process within a small area is indicated. Cooperation between physicists, engineers and physicians has led to the application of lasers in medicine. It is a prime example of the value of clinical application of basic science discoveries.
The safe use of any new medical instrument such as the laser requires that personnel be aware of the background principles and hazards involved. Laser is a form of electromagnetic radiation and strict adherence to safeguards against health hazards is essential.
Laser
Laser is an acronym for Light Amplification of Stimulated Emission of Radiation. The precursor of laser was Maser, a term coined by Nobel laureate, CH Townes, Microwave Amplification by Stimulated Emission of Radiation. In 1958, work was extended from microwaves to the visible light spectrum and led to the construction of the first ruby laser by Bell Telephone Laboratories. The output of early lasers was not well controlled until the technique of “Q” switching permitted all the energy of radiation to be stored in the laser and then released in pulses. Use of lasers in space technology led to further developments that have been incorporated into operating room lasers. In essence, a laser beam which is defined by wavelength, duration, energy and width of spot focused optics to direct a beam to a biological target. This effort results in ionizing radiation in situ, mechanical shock waves and vaporization of tissues by heat. The beam acts both as a scalpel and to coagulate blood vessels.
Characteristics
Lasers can be generated from solids, liquids or gases with resultant radiation of different wavelengths and biomedical properties. The materiasl used to generate the laser defines depth of vaporization and damage to tissues Table 1. Recently, fiber based lasers and distal chip flexible endoscopy have been added to facilitate a new type of surgery, especially in office based laryngeal procedures.1
Table 1
Some currently used laser sources
Laser Sources | |
|---|---|
Solids | |
Gases | |
Ruby (red beam) | Carbon dioxide (invisible beam) |
Neodymium-glass | Helium-neon (red beam) |
Yttrium-aluminum-garnet (YAG) | Argon (blue-green beam) |
Neodymium YAG | Krypton |
Erbium YAG | Nitrogen |
Atoms that can be excited to emit light waves are contained in the laser in long narrow tubes with mirrors at either end. External energy is provided initially to excite some of the atoms. The light wave emitted by these few atoms is amplified by stimulating other atoms to emit. A beam of wave is produced which develops tremendous energy by reflection from the mirrors. Finally, the radiation wave emerges from the partially reflective mirror as an intense directional beam of light. Laser beams are unique compared to other light wave beams because all other light or radiation is comprised of wave emissions from individual atoms independently of other excited atoms.
Laser characteristics include:
1.
A near single frequency of low band-width, i.e., an almost pure monochromatic beam.
2.
Precisely defined wave fronts. The point of impact can be the same as the wavelength.
3.
Enormous intensity and a high frequency of temporal and spatial coherence.
4.
A high plane of polarization and tremendous electromagnetic field strength.
Applications
Lasers have achieved many uses in medicine, mainly in surgery. They can be used to excise melanomas, tumors, dermatologic scars (tattoos, port wine stains) and also for cosmetic facial enhancement.2 As noted above, the new lasers are well suited for treatment of laryngeal epithelial diseases such as dysplasia and papillomatosis.1 Carbon dioxide lasers have been used successfully in the treatment of anogenital warts in children.3 In pediatric dentistry erbium lasers have been found effective for both dental and soft tissue treatments.4 Retinopathy of prematurity is amenable to diode laser therapy.5 Other applications have been in prostatic surgery and for complex eye surgery as in vitrectomy, retinal detachment and posterior capsulotomy.6 Perhaps one of the more innovative uses has been in the in utero coagulation of placental vascular anastomosis in the twin- to- twin transfusion syndrome.7 Other diagnostic uses include the application of laser spectroscopy to microanalytic techniques, Papanicolau smears and immunofluorescent techniques.
Because lasers are a source of coherent and monochromatic radiation that can be focused accurately with high intensity and essentially no blood loss, that are used in procedures that require precision. The laser accomplishes tissue excision by vaporization and at the same time seals small blood vessels. The use or the operating microscope ensures a bloodless operation with controlled depth of tissue removal. The carbon dioxide laser as an example emits an invisible wave of 10.6 μm which is absorbed within 0.2 cm of tissue surface.
Laser radiographs appear superior to conventional x rays and may be used in breast tumor imaging and occlusion of hemangiomas. An argon laser counter can determine a complete blood count and calculate derived parameters. A further use may be in caries prevention in dentistry.
Laser fiberoptics have been developed for operating room use. A further application is as an effective tool for mass communication in examination of patient records, test results and for teaching purposes. A helium- neon laser beam communication system has been used for central monitoring in an operating suite.
Laser Surgery Involving the Airway
Indications and Contraindications
Nd-YAG lasers may be used for debulking of tumors of the trachea, main-stem bronchi and upper airway by transmitting energy via fiberoptic cable through the suction port of a fiberoptic bronchoscope Procedures in and around the vocal cords and oropharynx may require the precision of the CO2 laser Patients with underlying cardiopulmonary disease may be unable to tolerate desaturation, hypoxemia, and hypercarbia associated with low concentrations of oxygen and interruptions in ventilation during laser surgery of the airway |
There are many types of lasers, each with specific indications. Neodymium-doped yttrium aluminum gradient (Nd-YAG) laser is the most powerful laser. It allows for a tissue penetration between 2 and 6 mm and is used for tissue debulking, particularly in the trachea, main-stem bronchi, and upper airway. The energy may be transmitted through a fiberoptic cable placed down the suction port of a fiberoptic bronchoscope. The Nd-YAG laser can be used in “contact mode” to treat a tumor mass, such as a papilloma (Fig. 1). Alternatively, the CO2 laser has very little tissue penetration and can be used where great precision is needed. One advantage of the CO2 laser in airway surgery is that the beam is absorbed by water, so minimal heat is dispersed to surrounding tissues. The CO2 laser is primarily used for procedures in the oropharynx and in and around the vocal cords. The helium-neon laser (He-Ne) produces an intense red light and can be used for aiming the CO2 and Nd-YAG lasers. It has a very low power and poses no danger to OR personnel or the patient.8
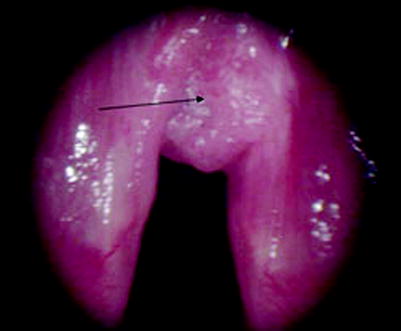
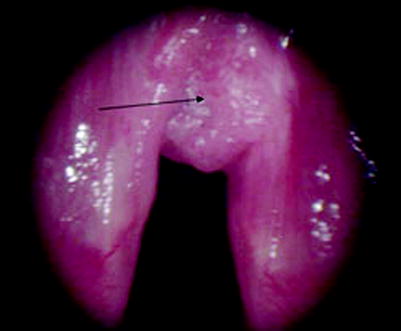
Fig. 1
Papilloma of the vocal cords
Because lasers are capable of igniting airway fires, use of high concentrations of oxygen and nitrous oxide is dangerous. Some patients with cardiopulmonary disease may not tolerate low concentrations of oxygen (at or just above room air) and the resultant desaturation and hypoxemia. In addition, interruptions in ventilation frequently result in hypercarbia and may result in arrhythmias. Prior to induction of anesthesia and surgery, a thorough history and physical help to identify patients who are at risk for complications during laser surgery of the airway and associated manipulations of oxygenation and ventilation.
Techniques
Patients with pathologic conditions involving the airway (i.e., mediastinal masses, tracheal stenosis) may be difficult to ventilate and/or intubate during induction of anesthesia Co-morbidities such as chronic obstructive pulmonary disease and coronary artery disease are present in many patients presenting for laser surgery of the airway and should be medically optimized pre-operatively Airway management for laser surgery of the larynx includes endotracheal intubation, intermittent apneic ventilation, and jet ventilation Short-acting opioids such as remifentanil or alfentanil in combination with a sedative-hypnotic (i.e., propofol) typically provide adequate depth of anesthesia for laser surgery of the airway and rapid emergence at the conclusion of surgery Post-operative pain control can generally be achieved with shorter acting opioids such as fentanyl and titrated to pain relief |
Pre-operative Management
Pre-operative management of patients requiring laser surgery for masses or tumors of the trachea, main-stem bronchi and upper airway involves careful attention to airway management. Airway compromise should be anticipated and a clear backup plan devised before the induction of general anesthesia. Patients with lesions in the mediastinum may be difficult to ventilate and/or intubate. Stridor suggests existing narrowing of the airway which may also compromise airway management. Inspiratory stridor indicates a supraglottic lesion, whereas, expiratory stridor suggests subglottic narrowing. Communication with the surgeon and careful planning are imperative during induction of anesthesia in this patient population. Furthermore, many patients presenting for laser surgery for lesions involving the airway are elderly and have a history of tobacco use. A history of chronic obstructive pulmonary disease suggests a need for a chest x-ray to rule out active pulmonary processes. Prior to induction, wheezing should be treated with bronchodilators. Coronary artery disease should be suspected in those at risk (age >65 years, male, family history, tobacco use, high cholesterol, hypertension, diabetes mellitus, obesity, and sedentary lifestyle.) Adrenergic response to airway manipulation should be anticipated and treated with beta blockade to decrease the risk of myocardial ischemia.9
Description of Technique
Laser surgery of the vocal cords requires the cords be immobile during laser firing. Adequate muscle relaxation is therefore important. The CO2 laser is generally used because of its ability to precisely vaporize tissue. The Nd:YAG laser coagulates deeper lesions and is used for tumor debulking.
Airway management for laser surgery of the larynx includes endotracheal intubation, intermittent apneic technique, and jet ventilation.
Endotracheal intubation with a small-diameter endotracheal tube (5.0–6.0 mm) or microlaryngeal tube allows for visualization of the larynx. The lowest possible FiO2 (less than or equal to 0.3 or 0.4) that assures adequate oxygenation is desirable. Nitrous oxide and a high FiO2 support combustion and should be avoided. Other precautions to prevent airway fires include filling the cuff with methylene blue normal saline and using a special laser endotracheal tube such as a Mallinkrodt Laser-Flex® or Xomed Laser Shield®. It should be noted that laser endotracheal tubes do not provide 100% protection for all laser types (Table 2).
Table 2
Characteristics of endotracheal tubes used during laser surgery of the airway
Type of tube | Non-reflective | Combustible | Kink resistant |
|---|---|---|---|
Polyvinyl chloride | + | ++ | − |
Red rubber | + | ++ | + |
Silicone rubber | + | + | − |
Metal | − | − | + |
Intermittent apnea technique allows tracheal extubation after a period of hyperventilation. The laser may be used during the time the patient is extubated for approximately 1–5 min prior to desaturation. A pulse oximeter must be accurate and always available. A disadvantage of this technique includes increased risk of airway edema and trauma.
Jet ventilation allows for ventilation without an endotracheal tube such as in treatment of some supraglottic and subglottic lesions. A ventilating laryngoscope is commonly used for supraglottic lesions. The jet flow should be aligned with the trachea and complete exhalation should be allowed prior to the next jet ventilation. By triggering the jet between laser firing, the vocal cords remain immobile. Complete muscle relaxation is essential with the use of jet ventilation. Complications include pneumothorax, barotrauma, and gastric distension.
Standard induction techniques may be used depending on the co-morbidities of the patient (i.e., rapid sequence intubation for those at risk for aspiration.) In general, minimal post-operative discomfort implies decreased need for narcotics intra-operatively. Short-acting opioids such as remifentanil (0.1–0.25 mcg/kg/min) or alfentanil (0.25–0.1 mcg/kg/min) may be used in combination with propofol (100–150 mcg/kg/min) to maintain adequate anesthetic depth while allowing for rapid emergence. As previously mentioned, adequate neuromuscular blockade is especially important in surgery involving the vocal cords.
In most cases, full recovery of airway reflexes should be obtained prior to extubation. In special circumstances, such as vocal cord surgery, the surgeon may request a smooth emergence involving deep extubation. In either case, gastric decompression prior to extubation is prudent, especially following the use of jet ventilation.
Post-operative Management
Use of short acting opioids such as intravenous fentanyl (25–50 mcg) as needed for pain control in the post-operative is usually adequate. Depending on the nature and invasiveness of the surgical procedure, longer acting narcotics such as morphine or dilaudid may be necessary to make the patient comfortable. There is risk of pneumothorax and barotrauma with jet ventilation. If suspected, a chest x-ray should be obtained.
Adverse Events
Factors contributing to the risk of airway fire during laser surgery include energy level of the laser, the gas environment of the airway, and the type of endotracheal tube A safe gas mixture of 25–30% oxygen and avoidance of nitrous oxide decreases the risk of airway fire during laser surgery Laser-resistant endotracheal tubes are designed to prevent fires associated with laser use The anesthesiologist and all members of the operating room team should remain vigilant in recognizing the early signs of airway fire (i.e., unexpected flash, flame, smoke, odors, discolorations of the breathing circuit) In the event of an airway fire, the endotracheal tube should be removed immediately and the flow of gases stopped followed by removal of burning materials and saline or water poured into the airway |
Side Effects/Complications
The most serious complication of laser airway surgery is fire. Airway fire may occur when an endotracheal tube is ignited. Several factors contribute to the likelihood of airway fire including the energy level of the laser, the gas environment of the airway, and the type of endotracheal tube. Oxygen and nitrous oxide both support combustion thus pose a fire hazard. If the patient is being ventilated with oxygen or nitrous oxide, the endotracheal tube emits a blow-torch type of flame that results in severe injury to the trachea, lungs, and surrounding tissue. Endotracheal tubes made of polyvinyl chloride, silicone, and red rubber have oxygen flammability indices of 26%. Wrapping the endotracheal tube with reflective tape still imposes a hazard in that kinking of the tube may occur, gaps may be present, and non-laser resistant tape may be inadvertently used.
Prevention and Treatment of Side Effects/Complications
The prevention of airway fires involving laser use begins with communication amongst the anesthesiologist, surgeon, and all members of the operating room team. Precautions should be taken to minimize the risk of an oxygen rich environment that would support ignition and combustion. To prevent fires associated with endotracheal tubes and laser use, laser-resistant endotracheal tubes have been developed. It is best to use an endotracheal tube that is designed to be resistant to a specific laser that may be used in surgery (e.g., CO2, Nd:YAG, Ar, Er:YAG, KTP). The tracheal cuff of the laser tube should be filled with saline and colored with an indicator dye such as methylene blue to alert the surgeon if he contacts the endotracheal tube. To minimize the risk of ignition, a safe gas mixture during laser surgery involving the airway is oxygen/air or oxygen/helium to achieve an oxygen concentration 25–30% or minimal oxygen concentration required to avoid hypoxia. Nitrous oxide should be avoided. Surgical drapes should be arranged to reduce the accumulation of oxidizers under the drapes. Gauze and sponges should be moistened prior to use near an ignition source.
The energy level of the laser is controlled by the surgeon and activation of the laser should be preceded by adequate notice. Safe use of laser in airway surgery includes intermittent and noncontinous mode at moderate power (10–15 W.) In addition, allowing time for heat dispersal and packing of adjacent tissues with moist gauze helps reduce the risk of airway fire.11 Precautions that should be taken to minimize the risk of airway fire include:
1.
Intubation with a laser resistant endotracheal tube resistant to the specific type of laser to be used
2.
Filling the endotracheal tube cuff with saline or an indicator dye such as methylene blue
3.
Requesting the surgeon to give adequate notice prior to activating the laser
4.
Reducing the concentration of oxygen to the minimum avoiding hypoxia
5.
Discontinuing use of nitrous oxide
6.
Waiting a few minutes after reducing the oxygen concentration before allowing laser activation
The anesthesiologist and members of the operating room team must be vigilant in recognizing the early warning signs of fire. Examples include unexpected flash, flame, smoke or heat, unusual sounds or odors, discoloration of the drapes or breathing circuit. If a fire occurs involving the airway, the anesthesiologist should immediately remove the endotracheal tube and stop the flow of all gases (Table 3). All flammable and burning materials should be removed from the airway and saline or water poured into the airway. Once the airway or breathing circuit is extinguished, mask ventilation should be established avoiding oxygen and nitrous oxide if possible. The removed endotracheal tube should be examined for fragments that might be left in the airway and bronchoscopy (rigid preferred) considered to assess injury and remove any debris. The patient’s status and plan for ongoing care such as admission to the intensive care unit, serial chest x-rays, arterial blood gases must be reassessed.11
1. Remove the endotracheal tube |
2. Stop the flow of all gases |
3. Remove flammable and burning materials from the airway |
4. Pour saline or water into the patient’s airway |
Anesthesia for Cutaneous and Cosmetic Laser Surgery
Indications and Contraindications
Cosmetic laser surgery is frequently used to minimize the signs of aging in areas such as periorbital and perioral creases Laser skin resurfacing can successfully treat scars related to acne and trauma, as well as, pre-cancerous lesions |
Laser skin resurfacing is used to treat a variety of skin conditions including acne scars, traumatic scars, and pre-cancerous lesions such as actinic keratosis. Cosmetic laser surgery utilizes a controlled burn to the facial skin to reduce the signs of aging, especially in the periorbital and perioral creases where previous cosmetic techniques were lacking.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree