ENUCLEATION AND EXENTERATION
John L. Wobig and Roger A. Dailey
There are several indications for removal of the human eye, such as phthisis bulbi, malignant tumors, and trauma beyond primary repair. Evisceration can also be performed instead of enucleation in many of these cases. It has been our experience (and that of others), however, that the incidence of post-operative complications and pain is significantly higher with evisceration. In addition, the cosmetic results following enucleation using newer implants such as hydroxyapatite and Medpor have been excellent. As such, evisceration is not performed any longer in our practice and will not be discussed in this book.
The enucleation procedure can be broken down into two main phases: the actual enucleation, and the implantation of some material inside the muscle cone to make up most of the lost volume. The remainder of the soft tissue volume loss is made up by the prosthesis. In our practice, the most common muscle cone implant placed is hydroxyapatite. Medpor is occasionally used but appears to have a higher exposure rate. In cases where bulbar conjunctival or fornix adequacy is an issue, a dermis fat graft is placed.
SURGICAL TECHNIQUE
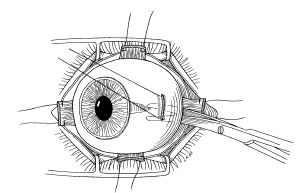
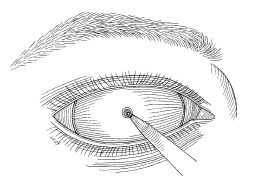
With the patient in a supine position under general anesthetic, a lid speculum is inserted. A retrobulbar block and local subconjunctival injection of anesthetic can be administered prior to initiating surgery but is not necessary unless intravenous sedation is used. A lid speculum is inserted and a 360 degree limbal peritomy is then performed. Following this, the four orbital quadrants between the extraocular muscles are entered with a blunt Stevens tenotomy scissors and the Tenon’s capsule is opened with a spreading motion (Fig. 18-1). The rectus muscles are then captured on a muscle hook and a double-armed 5-0 Vicryl (910 polyglactin) suture is placed near the insertion. The muscle can then be released from the globe utilizing a Wescott scissors (Fig. 18-2). All four rectus muscles are released in this fashion. The inferior oblique muscle and superior oblique tendon are generally not tagged but can be found and released at this point or after the optic nerve has been cut and the eye is on its way out. A traction suture is then placed through the sclera at the insertion of the medial rectus muscle on the globe, allowing for retraction laterally of the globe. With the eye in this position, a curved clamp can be placed behind the posterior pole of the globe. If the surgeon employs a strumming motion, the nerve can be identified and cross-clamped. Following this, the nerve is cut with a gently curved Metzenbaum scissors (Fig. 18-3). The eye is then removed and any attachments severed sharply. It is important to maintain adequate pressure in the muscle cone and orbit after removing the eye because hemorrhage into the soft tissues can make it difficult to place an appropriate-sized implant. Digital tamponade over 5 minutes or so will generally allow for hemostasis; however, bipolar cautery can be useful at this point to achieve excellent hemostasis. Post-operative orbital hemorrhage should be avoided because it increases the incidence of exposure of the implant.
HYDROXYAPATITE
Most adult orbits can easily handle an 18 or 20 mm implant. The implant should be oriented so that the natural channels are directed in an anteroposterior fashion. What will be the anterior portion of the implant is then slightly truncated and all sharp edges are taken down with a No. 15 blade (Fig. 18-4A). The donor sclera is then cut to fit and wrapped around the implant and held in place with a running 5-0 Vicryl suture (Fig. 18-4B). Four rectangular windows are then cut out of the sclera anterior to the equator in position to accept the four extraocular rectus muscles (Fig. 18-4C). The scleral wrapped implant is then placed deep into the muscle cone and the four rectus muscles are attached with the previously placed 5-0 Vicryl sutures (Fig. 18-5). The Tenon’s capsule is then closed over the implant in a running fashion using the 5-0 Vicryl, and the conjunctiva is then closed with a running stitch of the same material. A conformer or Natural Iris Conformer™ (Maloney’s Ocular Prosthetics, Portland, Oregon) is then placed in the fornix along with some antibiotic ointment. If the lids do not remain closed, or if swelling is a concern, one or two Frost sutures can be placed. An epidural catheter is then placed in a retrobulbar fashion to allow administration of 3 mL of Marcaine (bupivacaine). The catheter is left in place until the pressure patch over the operative eye is removed in 3 days.
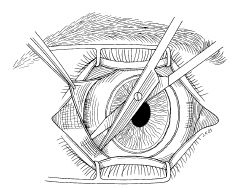
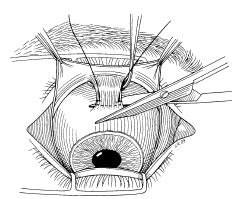
FIGURE 18-3 Severing the optic nerve.
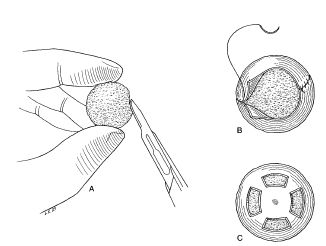
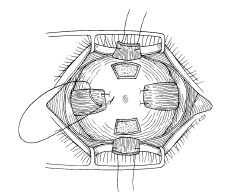
FIGURE 18-5 The scleral-wrapped implant is placed deep into the muscle cone. The four rectus muscles are attached with previously placed 5-0 Vicryl sutures.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree