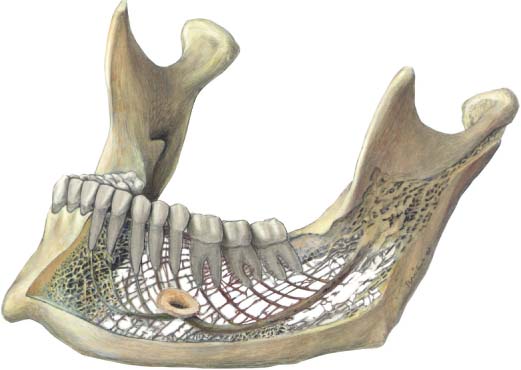
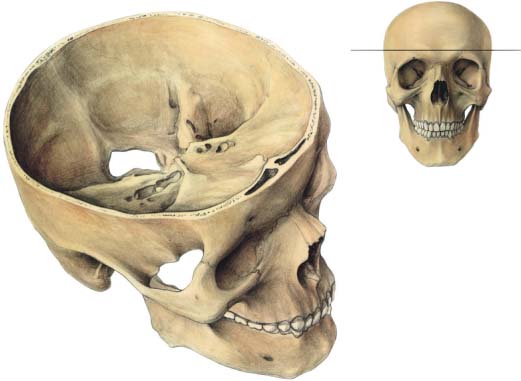
1 Anatomical Aspects and Biomechanical Considerations for the Body of the Mandible, the Midface, and the Cranium Monocortical miniplate osteosynthesis is based on precise anatomical considerations and extensive biological and mechanical experiments that have led to the development of specific instruments and hardware. Following innovative intraoral miniplate osteosynthesis (Michelet, Deymes, and Dessus, 1973), experimental work and clinical application have demonstrated that monocortical fixation by miniplates is strong enough to withstand the different strains created by masticatory forces (Champy et al., 1975; Champy et al., 1976a, b; Champy et al., 1977; Champy et al., 1978a, b; Champy and Lodde, 1976; Champy and Lodde, 1977; Jaeger, 1978). Because fixation is accomplished by anchoring the miniplates to the bone by means of screws, it is important to know both: • the regions where the bone provides the screws with a firm anchorage • the topography of the dental apices and inferior alveolar nerve, to avoid damaging them when inserting the screws The outer cortex of the body of the mandible has an average thickness of 3.3 mm; it is particularly strong and offers a good anchorage for the osteosynthesis screws. The cortical bone is thicker in the chin region and is reinforced laterally by the oblique line, which runs from the coronoid process to the molar region. In the symphysis region cross-sections of the mandible show the thickest cortex to be at the lower border; behind the third molar it is stronger at the upper border (Fig. 1.1). Near the alveolar process the thickness of the bone is variable; the anatomy of the tooth roots and the structure of the bone do not allow screw fixation in this region (Gerber, 1975). To avoid damaging the root apices, it is safe to place the screws away from the occlusal plane by a distance of at least three times the length of the crown of the tooth. The inferior alveolar nerve runs in the mandibular canal, from the lingula to the mental foramen, on a concave course. Measurements show that, from back to front, it runs ever closer to the outer cortex and to the lower border. At its lowest point it is 8–10 mm away from the basilar border of the mandible. Although the average thickness of the cortex in that region is 5 mm, it may be less than 3 mm in some cases. About 1 cm before the mental foramen, the canal turns upward and forward (Härle, 1977). The foramen lies approximately midway between the alveolar crest and the lower border of the mandible on a vertical line corresponding to the first or second premolar. It is important to remember that the mental foramen sometimes lies higher than the canine apex. Therefore, osteosynthesis in this region involves a certain risk of apical injury. Fig. 1.1 Lateral view of a mandible. The lateral and inner cortex of the body of the mandible is taken out. Fig. 1.2 Elective zones of miniplate osteosynthesis. Favorable regions are colored blue. The red zone is a region where microplates can be used. The green zone is a region where microplates or miniplates can be used. In most cases the mandibular canal surrounds the neurovascular bundle as a bony tunnel, but sometimes its bony structure is poorly developed. Repeated tests in freshly prepared mandibles have shown that the intrusion of a screw into the canal does not usually cause nerve injury, because the nerve moves away from the instrument (Gerber, 1975). Drilling the holes appears to be more dangerous to the nerve than inserting the screws. It should be noted that, with aging, the alveolar bone atrophies and the structure of the mandible is reduced to the two cortical layers. In edentulous patients the flat upper border of the mandible is composed of sclerous bone, giving poor anchorage for the screws. One should keep in mind that in children the mandibular body is occupied by dental germs. The alveolar bone is covered with attached mucosa. When a fracture occurs, the gum is often lacerated, exposing the mandibular bone to the risk of infection from the oral cavity if treatment is not instituted within 12 hours. During the first years of life, the blood supply of the mandible depends on the inferior dental artery (Cohen, 1960). Later, periosteal vascularization increasingly takes over. In the adult subject, as demonstrated by Bradley (1975), the blood supply relies entirely on the periosteum of the basilar process. This area should therefore be treated with care. Extensive periosteal stripping should be avoided to preserve the blood supply. For this reason a transmucosal rather than a transcutaneous approach is preferred. In the facial and cranial skeleton the thickness of cortical bone is variable. The use of miniplate osteosynthesis in cranial and midface surgery has been advocated by Loddé and Champy (1976), and Champy, Loddé, and Grasset (1977). Short miniscrews of 3 mm or 5 mm in length should be used in cranial surgery. Those areas where the cortical bone is thick and therefore suitable for osteosynthesis include the cranium, the nasal bone, the zygomatic bone, the orbital rim, the marginal rim of the piriform aperture and the zygomatic buttress (Mariano, 1978). Elsewhere the cortical bone that constitutes the walls of the various cavities is thin and does not provide a very solid anchorage for osteosynthesis screws, and is only suitable for fixation with microscrews and microplates (Fig. 1.2). The frontal bone ranges from 4 to 9 mm in thickness. The upper orbital margins are particularly well-suited for plate placement, but care should be taken to localize the contours of the frontal sinus. Bone thickness allows placement of 5 mm long screws without risking dural penetration. The parietal bone also provides adequate thickness for fixation with screws of 3 mm in length. The frontozygomatic process, which resembles a triangular prism, is made of compact cortical bone and provides an excellent area for fixation of cortical screws. It is covered with a periosteum that is easily elevated, except at the frontomalar suture. The lateral orbital rim extending to the zygomatic arch provides sufficient bone for screw fixation. The eye should be protected during the operation by using an appropriate retractor. After Champy et al., 1975, the anterior cerebral fossa can be avoided; its deepest point is located 16–20 mm above the frontomalar suture, or 5 mm above a horizontal line tangential to the upper orbital margin (Fig. 1.3). Fig. 1.3 Localization of the anterior cerebral fossa. Its deepest point lies 16–20 mm above the frontomalar suture, 5 mm over the tangential line of the upper orbital margin. The lower orbital rim is also an area of thick cortical bone. However, because neither muscular force nor any strain is exerted on it, its fixation with a plate seems unwarranted. If isolated fragments require immobilization, absorbable ligatures or microplates are mechanically sufficient. The maxilla has only two buttresses made of compact and strong bone: the lateral inferior aspect of the piriform aperture (medial or nasomaxillary buttress), and the lateral or zygomatic or maxillary buttress. The importance of these pillars or buttresses was described in 1928 by Sicher and Tandler, by de Brul (1970) and more recently by Manson, Hooper, and Su, 1980. The anterior wall of the maxillary sinus is thin and less suitable as a support for miniplates. Finally, remember that many cavities exist in this area, some of which contain organs that must be preserved, such as the dura, the eyes, and the dental roots. The walls of the frontal, maxillary, and ethmoid sinuses, the nasal fossae, and the buccal cavity are generally thin and fragile. Protrusion of screws into these cavities should be avoided, as there is a risk of causing infection, particularly in the frontal sinus and the nasal cavity. Physiology is the scientific study of the properties and functions of tissues in living beings. Mechanics is the scientific study of the equilibrium of forces and the movements that generate them. Biomechanics is the study of biological phenomena with the objective of proposing explanations or therapeutic solutions for such phenomena (e. g., fractures). In practice it consists of an amalgamation of knowledge from engineers and biologists.
Anatomical Considerations
The Mandible
The Midface and the Cranial Bones
Biomechanical Principles
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree