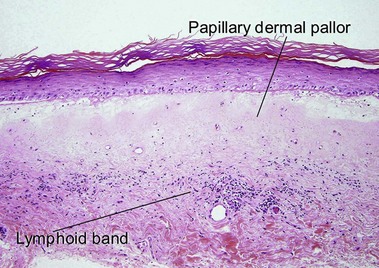
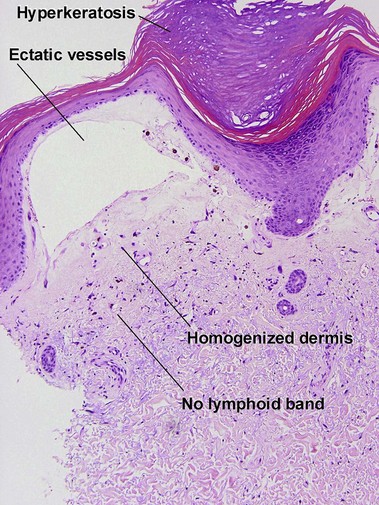
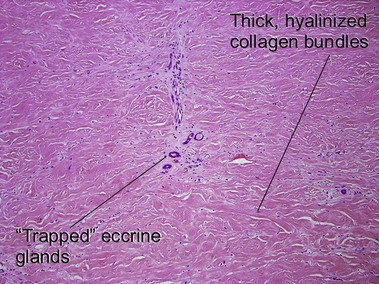
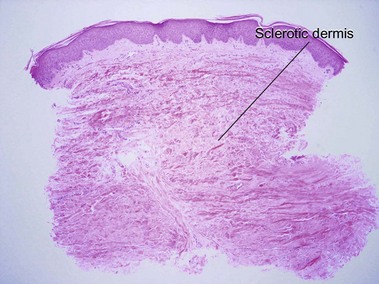
Chapter 13 Lichen sclerosus may involve skin or mucosa. Follicular plugging is common, and the plugs may resemble comedones clinically. The epidermis is commonly atrophic and the rete pattern is commonly effaced; however, scratching may produce pseudoepitheliomatous hyperplasia, especially in vulvar lesions. Squamous cell carcinoma rarely develops in long-standing genital lesions of lichen sclerosus and must be distinguished from pseudoepitheliomatous hyperplasia. Papillary dermal edema may produce a subepidermal bulla. Vacuolar interface dermatitis and pigment incontinence are common. Epidermotropic lymphocytes may be hyperchromatic and may mimic mycosis fungoides (Table 13.1). The differential diagnosis also includes radiation dermatitis and morphea. Table 13-1 Features of lichen sclerosus and chronic radiation dermatitis There is typically hyperkeratosis and epidermal atrophy with effaced rete that may alternate with hyperplasia. Stellate cells with large nuclei are usually present (radiation fibroblasts). The eccrine glands are atrophic and the pilosebaceous structures are absent; however, the arrector pili muscle may survive. The dermal collagen is hyalinized. Radiation elastosis may resemble solar elastosis but extends into follicular fibrous tracts. The superficial blood vessels are dilated, whereas the deeper vessels have thick walls. Scleroderma encompasses a group of diseases. Localized cutaneous disease may present as morphea or linear scleroderma (including en coup de sabre). In addition to cutaneous lesions, Raynaud’s phenomenon and variable organ involvement characterize diffuse systemic scleroderma and limited systemic scleroderma (CREST). Although the histologic features are similar, morphea is usually more inflammatory and lacks the intimal thickening and luminal obliteration of vessels seen in systemic scleroderma.
Alterations in collagen and elastin
Lichen sclerosus (et atrophicus)
Feature
Lichen sclerosus
Chronic radiation dermatitis
Compact red stratum corneum
Yes
Yes
Superficial dermal pallor
Yes
Yes
Epidermal atrophy
Variable
Variable
Follicular plugging
Common
Rare
Vacuolar interface dermatitis
Yes
No
Lymphoid band
Yes
No
Pigment incontinence
Common
Usually absent
Superficial dermal vessels
Normal to slight dilatation
Widely ectatic
Radiation elastosis
No
Yes
Adnexal structures
Present
Absent
Large stellate fibroblasts
No
Yes
Deep dermis
Normal
Sclerotic
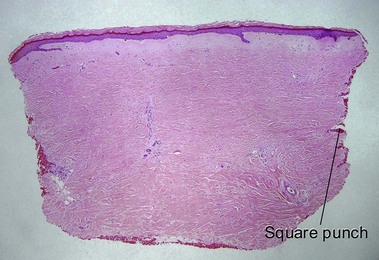
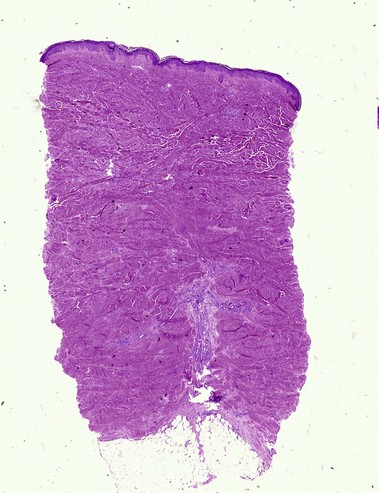
Shape of punch biopsy
Tapered
Square
Chronic radiation dermatitis
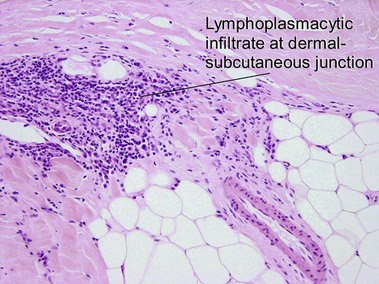
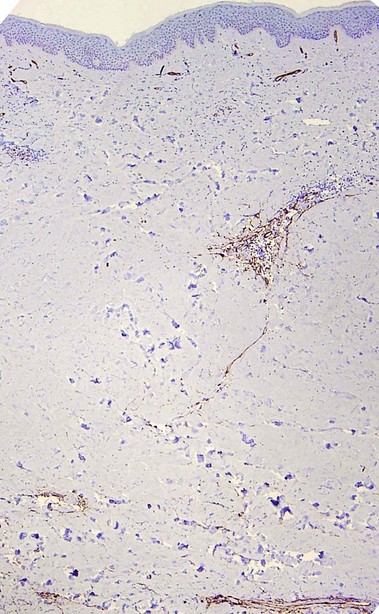
Morphea/scleroderma
Plastic Surgery Key
Fastest Plastic Surgery & Dermatology Insight Engine