Chapter 32. Alloplastic Volumizing Augmentation of Midface and Mandible Sections
Edward O. Terino, MD, FACS
ALLOPLASTIC AUGMENTATION
Six Basic “Principles” Applied to All Alloplastic Volume Alterations of Any Aspect of Facial Anatomy
1. Purpose. The purpose of volume alterations aligns completely with the optimum goal of aesthetic facial surgery, that is, the 3-dimensional restructuring of facial form and balance.
2. Principles of aesthetics. Alloplastic volume alterations are highly effective in establishing the facial balance, which results from the symbiotic interrelationship of volume differentials and deficiencies within the zones of anatomy and interrelate the aesthetic regional segments of the face (Fig. 32-1). Correction of volume deficiencies in specific regions and zones constitute aesthetic balance.
Figure 32-1 New aesthetic perception of a face: upper two-thirds and lower one-third.
3. Predictability. Alloplastic implants do not change over time. The materials from which they are made remain stable. Moreover, implants are fixed in location by encapsulating fibrosis, which constitutes the normal physiologic response.
4. Precision. Because alloplastic implants are volume devices with a noncompressible shape and form, their size and location are extremely critical. Small changes in the measurement, shape, and anatomic location of the facial implant create a much greater difference than 2-dimensional tightening of autogenous elastic facial tissues. This fact becomes more valid as aging and attenuation of the elastic subcutaneum occurs.
5. Permanence. The shape, size, and configuration of facial contours produced by alloplastic implants remain permanent. But depending on the material used, regional contours can be altered readily by an easy implant exchange. This is particularly true when using silicone rubber implants. Moreover, if the changes are considered undesirable, removal of the implants in most instances produces complete reversibility to the previous natural state without deformity or disfiguration.
6. Practice. Practice is absolutely necessary to understand fully the remarkable aesthetic changes that can be realized from alloplastic augmentation. The artistic expertise to use facial implants with predictability and precision can only be gained from experience. The technical aspects of the surgery are relatively simple and very easy for a novice to learn.
Indications
Alterations of facial volume and contour are easily predictable by using the practical model for anatomic analysis by skeletal facial zones (Fig. 32-2).
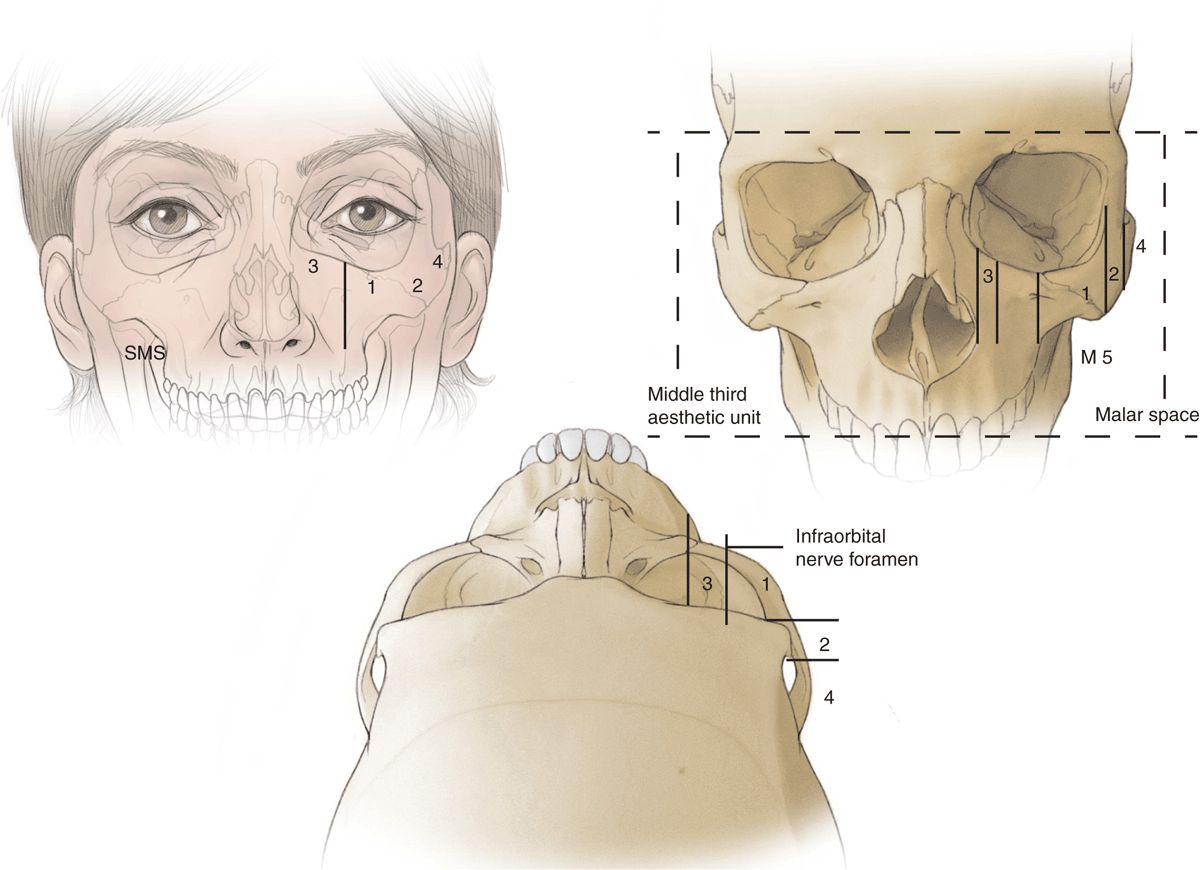
Figure 32-2 Anatomic facial contour zones of midface.
Zone 1
The implant is placed on the major body of the malar bone, producing a high strong malar bone contour. This is most frequently useful for young men who desire a well-defined sculpture appearance. It is also useful in young women who desire a more exotic look.
Zones 1, 2, and 3
Volumization of the lateral and suborbital region in patients who have a hereditary or posttraumatic deficient maxilla with suborbital and malar flattening. This can extend from the medial canthus to include the major body of the malar bone.
Zone 2 Procedures
Widening in the middle third of the zygomatic arch, which produces greater width to the upper third midface aesthetic segment. This can be desirable in someone with a narrow upper face.
Zone 3
Increased volume and shape in the paranasal tear trough and the suborbital areas. Volume deficiencies in these areas appear as a tired, hollow appearance. Isolated tear trough suborbital deficiencies may also be corrected.
Zone 4
The posterior third of zygomatic arch, according to the perception of the authors, never needs augmentation for aesthetic purposes. Surgical dissections in this zone could produce temporomandibular joint symptoms or permanent damage.
Malar Zone
The lower half of the midface can be called the submalar (SM) region, which exists beneath the lower border of the malar bone and lies on the surface of the masseter muscle. It is often deficient because of aging atrophy or heredity factors. Accentuation or contour improvements in this area are the most frequent reason for implants to be used. Submalar aging changes of the face as a result of facial atrophy causes a dissipated, emaciated appearance and the loss of youthful midfacial fullness.
Preoperative Preparation
The overriding most important principle with all allo-plastic facial implant surgery is to spend sufficient “communication time” with a patient to achieve a complete understanding of their contour goals and expectations. These must be understood with certainty and precision.
A computer imaging program is indispensable along with the “homework assignment” of having patients bring photographs of friends, family, earlier periods in their life, as well as pictures of models, actresses, and the like, who have contours in the malar midface region they would like to emulate (“ideal scene”).
The limitations, as well as possible complications from the surgery, must be thoroughly discussed, as well as alternative methods of treatment such as injectable fillers, autologous fat transplants, and upper midface suspension techniques.
Anesthesia
Malar midface implant augmentation techniques require general anesthesia. Local anesthesia and monitored sedation are usually avoided because of the possibility of aspiration of blood or saliva. Copious injection of local anesthesia into the anatomic dissection areas to be implanted facilitates optimum hemostasis and easy anatomic planar dissection. Injected into each implantation site is 20 to 30 mL of lidocaine 0.25% with adrenaline 1:600,000.
Position and Markings
After using computer imaging and photos to decipher the patient’s beauty ideal, both the patient and surgeon agree on a malar or submalar midface contour shape. The specific implant size is chosen on the morning of surgery. The patient is seen first in an examining room where the computer images and “game plan” are reviewed with the patient. A marking pen is used to outline the lateral orbital rim and the malar zygomatic bone in its entirety. The patient is asked to smile, which facilitates the marking of the submalar space below the lower border of the malar bone. The regional zones 1 through 4 and SM (submalar space) are also labeled on the face.
A variety of implant sizes and shapes are then demonstrated and discussed with the patient (Fig. 32-3). Together, a mutual agreement is reached about the exact implant location, size, and shape, which is determined by the computer image that was created, as well as from the photographs that the patient has brought in. Most commonly (99%), 4-mm thick implants in small, medium, large, and extralarge sizes are selected. The exact one is chosen by the implant surface area, which can be observed by placing an implant on the face within the confines of the malar-submalar-zone markings.
Figure 32-3 Anatomic-style implants used to imitate natural bony and soft-tissue contours in malar-midface and permeable regions.
Details of Procedure
After 30 years of experience and several thousand midface augmentations, the senior author has found that 2 approaches work best: (a) intraoral and (b) lower-eyelid subciliary and occasionally transconjunctival. It is also possible to put them through the superficial musculoaponeurotic system (SMAS) fascia in the zygomatic region underneath a facelift flap through a small 1-cm aperture directly down onto the bone in the lateral zone 1 area where it is certain that there are no branches to any important motor nerves.
Intraoral Approach
This approach has the least morbidity and is the easiest to perform. A 1-cm oblique incision is made through only the mucosa over the canine tooth with a 1-cm lateral extension. This creates an L-shaped incision. A 3-mm elevator is thrust directly through the incision beneath the orbicularis oris musculature and onto the inferior maxillary buttress, approximately 2 cm above the gumline over the third canine tooth. A 10- to 13-mm spatula elevator is used to dissect on the subperiosteal plane up the maxillary buttress to the major point of prominence where the masseter muscle and tendon arise from the anterior malar bone. The dissection is extended posteriorly on the bone to dissect the soft tissues from the major body of the malar bone (zone 1) and lateral over the midzygomatic arch (zone 2) (Fig. 32-4).
Figure 32-4 Minimally invasive intraoral dissection for placing midface implants.
The dissection is oblique and extends laterally as it is carried superiorly on the maxillary buttress, making it a safe distance from the medial infraorbital foramen and nerve. When a tear trough or suborbital tear trough malar implant is inserted, the dissection must extend medially to carefully visualize and isolate the infraorbital nerve trunk and the foramen. In such cases, the dissection is carried above the infraorbital nerve foramen and along the infraorbital rim to the junction of the nasal bone and the maxilla.
By dissecting only on the subperiosteal bony surface, injuries are avoided to the zygomaticus major and minor, as well as the frontalis musculature. Also, significant muscle damage may stimulate capsular contracture or pain during the healing process.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree