10 Aesthetic Concerns in Skin of Color Patients
Summary
Men of color represent a diverse segment of the male patient population with specific aesthetic concerns and unique considerations. This cohort includes, but is not limited to, individuals of African, Asian (East and South), Hispanic/Latin American, and Middle Eastern ancestry who are more likely to have Fitzpatrick skin phototypes IV to VI. Despite the considerable size and projected growth of this population, there is a paucity of published literature or research studies addressing aesthetic concerns in men with skin of color. Understanding the needs of ethnic skin is critical to obtaining good patient outcomes in the field of aesthetic dermatology. Although there is an appreciation for the fundamental differences between different Fitzpatrick skin types, there is a distinct lack of research and management guidelines specifying differences in ethnic skin. This chapter will serve as an introduction and guide to evaluating, assessing, and treating the unique and diverse aesthetic concern in men of color.
Keywords: aesthetics men skin of color procedures follicular disorders
10.1 Background
10.1.1 Anatomy and Physiology of Ethnic Skin
Differences in the skin structure and physiology of ethnic skin require differences in safety considerations and potential efficacy. The care and management of aesthetic skin concerns in men of color necessitates an understanding of the physiologic differences of ethnic skin, and the resultant treatment modifications required to ensure the appropriate settings for energy-based devices, techniques for injectable fillers, and dosages for prescription medications. In the field of aesthetics in particular, according to the latest data by the American Society for Aesthetic Plastic Surgery, ethnic minorities (Hispanics, African Americans, Asians) are the quickest growing fraction of the aesthetic procedure market.1 From 2017 to 2018, the number of ethnic patients seeking minimally invasive cosmetic procedures increased three times more than the number of Caucasians at a global level. Reasons for this exponential growth include increased exposure and access to procedures, targeted advertising, and socioeconomic advancement of certain cohorts in these populations. Ethnic patients have unique natural features and cosmetic concerns that require a thorough understanding by the dermatologists and cosmetic surgeons who will treat these patients.2 Further, ethnic populations have unique cultural beliefs and ideologies that need to be taken into consideration, and physicians trained to practice only on white patients will be ill equipped to offer optimal clinical care to patients of color. All of this underscores that it is critical for physicians treating aesthetic concerns in ethnic men to anticipate potential differences in skin response, recognize therapeutic limitations, and appreciate patient concerns.
The amount of epidermal melanin is the most apparent difference in individuals of color (Table 10.1). Whereas skin of all races and ethnicities contains the same number and distribution of melanocytes, individuals with darker skin have melanocytes that produce larger melanosomes that are more singly dispersed and contain greater quantities of melanin. Moreover, the melanin contained in the melanosomes of darker skinned individuals undergoes a slower rate of degradation.3 However, melanocytes in those with darker complexions often show a labile, exaggerated response to cutaneous injury.4–7
Table 10.1 Common Aesthetic Concerns in Men with Skin of Color
Postinflammatory hyperpigmentation |
Melasma |
Other dyschromia |
Dermatosis papulose nigra |
Textural irregularities (e.g., enlarged pores, roughness) |
Oily skin |
Acne scars |
Hypertrophic scars/keloids |
Pseudofolliculitis barba |
Acne keloidalis nuchae |
Rhytides |
Hair loss |
Several regulatory factors are involved in these differences; notably neuregulin 1 (NRG1) that accelerates the production and pigmentation of melanocytes has been shown to be expressed and secreted in higher levels by fibroblasts and keratinocytes of darker skin types compared to lighter skin types.8 Moreover, the RAB27A melanosome transport molecule has been shown to be expressed in higher levels in darker skinned individuals.9 As melanin provides photoprotection from damaging ultraviolet (UV) light, darker skin is less susceptible to photoaging, which allows the epidermis and dermis of those individuals to retain their original structure throughout the aging process to a greater extent compared to lighter skinned individuals. Transmission of UVA light through the epidermis is 17.5% in pigmented skin and 55.5% in Caucasians, whereas the transmission of UVB through the epidermis is 5.7% for pigmented skin compared to 29.4% for Caucasians.10
Aside from pigmentation, the structure and function of the epidermis and dermis are different between the various ethnicities. The stratum corneum of black skin contains a greater number of corneocyte layers, with each layer presenting increased intracellular cohesion and compactness compared to white skin. Moreover, the content of lipids in the stratum corneum was shown to differ between ethnicities, with the cholesterol-to-ceramide ratio being the highest in Asians, intermediate in Caucasians, and lowest in African Americans.11,12 Corneocyte size does not differ between skin of different ethnicities, but higher levels of desquamation have been noted in black skin compared to white skin (Table 10.1).13
Transepidermal water loss (TEWL), which refers to the total amount of water vapor lost through the skin and related appendages under nonsweating conditions, has been shown in some studies to differ between racial/ethnic populations, with Asians having the highest amount of TEWL after tape stripping. Differences in the skin hydration and pH of different ethnicities have yet to be determined due to lack of consistent parameters and results across various clinical studies.14–16
Hair structure and biology also differ between various ethnic groups. Asian, Caucasian, and African hairs exhibit distinct characteristics in density, diameter, shape, mechanical properties, and composition. Hair of African origin is spiral, with frequent twists that have random reversals in direction, pronounced flattening, and irregular diameter.17 African hair also exhibits increased dryness, lower moisture content, less total sebum, and increased fragility due to decreased tensile strength compared to Caucasian hair.3 Asian hair has the greatest diameter with circular geometry, and hair follicles that are more metabolically active than other ethnicities. Caucasian hair is intermediate in diameter and shape and presents the greatest tensile strength among the ethnic groups. In terms of content, keratin and other proteins are similar across the various ethnic groups (Table 10.1).18
Due to the interplay between structural, functional, and cultural factors, the frequency of dermatologic and aesthetic concerns varies by racial/ethnic population.1,20,21,22 Aesthetic concerns that disproportionately affect men with skin of color include disorders of hyperpigmentation, aesthetic sequelae of follicular disorders, dermatosis papulosa nigra, and keloids or hypertrophic scars.22,23 In addition to these, there are concerns that are prevalent across all populations but may have unique considerations in men of color. A comprehensive list of the range of common aesthetic concerns in men with skin of color is presented in Table 10.1.
Minimally invasive treatments are essential tools in the management of leading aesthetic concerns in men of color. The most common minimally invasive procedures used to address aesthetic concerns in male patients with skin of color are listed in Table 10.2. As a result of structural and functional characteristics, performing aesthetic procedures in this patient population is associated with a higher risk of complications, most notably postinflammatory pigment alteration and hypertrophic scarring or keloid formation. However, with careful selection of device or peeling agent, use of conservative treatment parameters, and judicious pre- and posttreatment precautions, minimally invasive procedures can be performed safely and effectively in men of color.
Table 10.2 Common Aesthetic Procedures in Men with Skin of Color
Chemical peels |
Laser hair removal |
Electrodessication |
Nonablative laser resurfacing/photorejuvenation |
Botulinum toxin |
Soft tissue fillers |
Hair restoration (e.g., transplantation, platelet-rich plasma) |
10.2 Managing Hyperpigmentation
Hyperpigmentation is among the leading aesthetic concerns in men of color. It is frequently seen as a sequela of inflammatory disorders (e.g., acne, atopic dermatitis, psoriasis, etc.), a primary pigmentary disorder (e.g., melasma, lentigines, photo-induced hyperpigmentation, maturational hyperpigmentation, etc.), or as a complication of dermatologic procedures and treatments. Minimally invasive procedures including chemical peels,24–29 fractional lasers,30,31,32,33,34 Q-switched lasers,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49 picosecond lasers,50,51,52,53,54,55,56,57,58 and microneedling59,60,61,62,63,64,65—typically in conjunction with topical skin lightening agents—have been used successfully on patients with higher skin phototypes and are a mainstay in the overall management of hyperpigmentation. Minimally invasive procedures contribute to the treatment of hyperpigmentation either by increasing penetration of topical skin lightening agents (e.g., chemical peels, fractional lasers, and microneedling) or by removing excess pigment (e.g., fractional lasers, Q-switched lasers, picosecond lasers, and chemical peels). Combining multiple modalities is often necessary to achieve the most efficacious results, but must be done with caution as excessive epidermal and dermal injury associated with the above procedures can result in iatrogenic dyspigmentation.
Although Q-switched lasers have been widely used in East Asian skin types (up to skin phototype III), their safety in more darkly pigmented individuals (e.g., skin phototypes IV–VI) is limited due to a higher rate of dyspigmentation—including irreversible guttate hypopigmentation. In a Thai study of men with melasma, five weekly 30% glycolic acid peels combined with weekly low-fluence Q-switched (LFQS) neodymium:yttrium aluminum garnet (Nd:YAG) laser demonstrated greater improvement in melasma than weekly glycolic acid peels alone. However, relapse rates were high and dyspigmentation associated with LFQS laser was observed. In a U.S. study involving melasma patients with skin phototypes II to V, monthly LFQS Nd:YAG lasers in combination with microdermabrasion and topical skin lightening agents resulted in significant improvement without treatment-associated dyspigmentation.66 As such, careful patient selection (favor lighter/intermediate skin types), lower frequency of treatments (monthly vs. weekly), lower fluences (e.g., 2 laser passes at 1.6–2.0 J/cm2),67 and combination of skin lightening agents are advised when considering LFQS in the treatment of melasma.
Low-energy 1,927-nm nonablative fractional laser has emerged as a safe and effective modality for treating hyperpigmentation in skin phototypes IV to VI. Two studies have included patients with higher Fitzpatrick skin phototypes (up to VI) with favorable results.30,68 This technology has the advantage of being able to extrude dermal pigmentation and enhance penetration of topical skin lightening agents while maintaining a very low risk safety profile.
10.2.1 Chemical Peels
Chemical peeling is a versatile minimally invasive procedure that plays a key role in the management of a broad range of aesthetic concerns in men of color (Table 10.3). They are particularly useful as an adjunct in the treatment of hyperpigmentation (in combination with topical skin lightening agents) and for the improvement of textural irregularities such as the appearance of enlarged follicular openings. They are also an effective approach to overall skin rejuvenation in the context of photoaging or for the purpose of skin care maintenance—enhancing radiance, reducing dyschromia, and improving texture.
Table 10.3 Best practices for performing laser/light based procedures in men of color (modified from Alexis AF, British Journal of Dermatology, 2013;169(3): 91–97)1
•Laser Wavelength–consider chromophore (especially risk of absorption by epidermal melanin); longer wavelengths associated with less epidermal absorption and therefore greater safety in patients with higher skin phototype |
•Laser treatment parameters–employ settings that minimize extent of epidermal and dermal injury (typically more conservative than in SPT I–III, often requiring a greater number of sessions), e.g., lower fluences and longer pulse durations for laser hair removal; lower treatment densities (microthermal zones cm2) for fractional laser resurfacing |
•Pre- and post-treatment sun protection (sun-protective behaviors, broad-spectrum sunscreen SPF ≥ 30) |
•Consider pre- (≥ 2 weeks prior) and post treatment bleaching agents (e.g., hydroquinone 4% cream) |
•Judicious epidermal cooling, e.g., slower treatment speeds when using lasers with contact cooling; pausing between passes of resurfacing lasers to reduce bulk heating; ice packs post-procedure |
•Consider topical corticosteroids post-treatment (to reduce inflammation), especially when significant post-procedure erythema or edema noted |
1Alexis AF. Lasers and light-based therapies in ethnic skin: treatment options and recommendations for Fitzpatrick skin types V and VI. The British journal of dermatology, 2013;169 (3):91–97. |
Superficial peeling agents are preferred for safety reasons—given the higher risk of dyspigmentation and scarring from medium and deep peels in patients with skin of color. Salicylic acid and glycolic acid peels are the most widely utilized, but other suitable peeling agents include mandelic acid, Jessner’s peel, and low-concentration trichloroacetic acid (e.g., 15% TCA). In a recent retrospective study, the overall complication rate of superficial chemical peels in skin phototypes III to VI was 3.8%.69 Key strategies to improving outcomes when performing chemical peels in male patients with skin of color are summarized in Table 10.4. Avoidance of over-application or, in the case of peels requiring neutralization, prolonged time of application is important for minimizing the risk of complications. As such, judicious application and close observation for impending signs or symptoms of irritation are of paramount importance.
Table 10.4 Best practices for performing chemical peels in men of color
•Utilize superficial peeling agents (e.g. glycolic acid 20-50%, salicylic acid 20-30%, mandelic acid 40%, trichloroacetic acid 15%) |
•Discontinue topical retinoids or exfoliate skin care procedures (e.g., exfoliating masks, mechanical brush cleansing, etc.) at least 7 days prior to chemical peel |
•Monitor patient closely during chemical peel |
•Customize number of layers applied and duration of application according to individual patient tolerability |
•Utilize portable fan and cool compresses to reduce stinging/burning |
•Neutralize or abort peel in areas demonstrating signs or symptoms of irritation during peel |
•Consider pre- and post-treatment topical skin lightening agents (for reduced risk of iatrogenic hyperpigmentation and enhanced efficacy in the management of hyperpigmentation) |
10.2.2 Laser Treatments
Nonablative fractional lasers can be used for a broad range of aesthetic indications in men with skin of color.70,71 The 1,550-nm erbium-doped fractional laser has been used extensively in patients of color72,73,74,75 and is particularly useful in the treatment of acne scarring, textural irregularities, and features of photoaging (Fig. 10.1). Postinflammatory hyperpigmentation (PIH) is a significant risk but can be managed by conservative treatment parameters—most notably, a lower range of treatment densities, pre- and posttreatment hydroquinone, as well as strict sun protection.
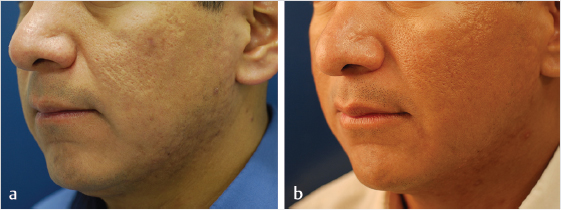
Fig. 10.1 A Hispanic man with acne scarring before (a) and after (b) laser resurfacing with 1550-nm erbium-doped fractional laser.
Other resurfacing technologies with broad applications in men of color include the microsecond pulsed Nd:YAG 1,064-nm laser71,76,77 and picosecond lasers.51,52,78 Submillisecond (300- to 650-microsecond) pulsed Nd:YAG can be used for the treatment of acne scars, keloids/hypertrophic scars, acne, dyschromia, and photoaging in patients of color. This approach has the advantage of being safe on all skin types and not requiring pretreatment anesthetic. However, multiple treatments are generally required to achieve clinically meaningful results. The 755-nm picosecond laser with the diffractive lens array (DLA) has been studied in the treatment of unwanted scars, pigmented lesions, and striae in patients with skin of color (Fitzpatrick skin phototypes IV–VI). Self-limited erythema and hyperpigmentation were the most common adverse events.51
Resurfacing with fractional radiofrequency (RF) has recently been demonstrated in a study involving 35 subjects with skin type VI who received three sessions of facial treatments, 4 weeks apart using a fractional RF device with 24-pin coated tip.79 Safety and efficacy in the treatment of wrinkles, acne scars, and overall appearance were observed.
10.3 Laser Hair Removal
Long-wavelength lasers in the near-infrared spectrum (especially the 800- to 810-nm diode and 1,064-nm Nd:YAG laser) have revolutionized the treatment of follicular disorders with aesthetic sequelae in men of color such as pseudofolliculitis barbae80,81,82,83,84,85,86,87,88,89,90,91 and acne keloidalis nuchae.92,93,94,95,96 Laser hair removal has also been shown to be effective as an alternative therapy for dissecting cellulitis of the scalp97,98 and hidradenitis suppuritiva.99 Whereas the 755-nm alexandrite laser has been used on lighter complexioned individuals with Fitzpatrick skin phototypes III to V,82,94,100 the 800- to 810-nm and 1,064-nm Nd:YAG laser is preferred for intermediately pigmented phototypes IV to V and richly pigmented phototypes V to VI, respectively, based on their risk-to-benefit ratio. In a study comparing Er:YAG laser resurfacing to long-pulsed Nd:YAG laser for the treatment of acne keloidalis nuchae in Egyptian men, both groups experienced a significant reduction in papules and plaque size, whereas a significant decrease in plaque count was only seen in the Er:YAG group.93 When using laser hair removal in men of color, utilizing lower fluences, longer wavelengths, and efficient epidermal cooling are key to maximizing safety. For millisecond pulsed lasers, the use of longer pulse durations are recommended for higher phototypes with richly pigmented skin in order to facilitate epidermal cooling and thereby minimize risk of pigmentary complications.
10.4 Injectable Fillers and Neuromodulators
10.4.1 Approach
The restoration of a youthful male face to combat the age-related loss of skeletal, muscle, and fat compartment volume is increasingly achieved with noninvasive procedures such as fillers and neuromodulators. The overarching goal for all patients, regardless of their gender or ethnicity, is to achieve harmonization in facial topography and rejuvenation. The aging process, however, affects different ethnicities distinctly, and different ethnicities have distinct structural characteristics that affect facial treatment planning. For example, individuals of African American origin, aside from having relative intrinsic protection against photoaging, have a thicker dermis and do not experience sagging, rhytids, and facial tissue ptosis to the same degree as their Caucasian counterparts. Signs of aging in these patients are more evident in the periorbital, perioral, and midface region and less on the upper third of the face. Patients of Asian origin present with a wide bitemporal, bizygomatic width, shorter face, and low projection of the midface. They have flatter, broader foreheads, retrognathia, and microgenia, and the aging process typically results in disharmonies in the lower third of the face. Aside from structural facial differences, ethnic patients are also susceptible to discoloration and scarring; thus, when treating them with injectable agents such as soft-tissue fillers and neuromodulators, the technique needs to be modified to minimize risk of these complications.
10.4.2 Procedure
Several types of fillers, notably hyaluronic acid (HA), calcium hydroxyapatite (CaHa), and poly-L-lactic acid (PLLA), have been used safely and effectively in individuals of diverse ethnic backgrounds.101–103 Strategies to minimize the risk for hyperpigmentation (PIH) after soft-tissue filler injection include longer, slower injection times and avoidance of a multiple puncture technique. In a clinical trial of 150 patients (skin types IV–VI) evaluating the safety and efficacy of hyaluronic fillers, 13% of multiple puncture techniques resulted in hyperpigmentation compared with 2% of linear threading.102 Moreover, due to the presence of larger, multinucleated fibroblasts, ethnic skin is 3 to 18 times more prone to the development of keloid formation; physicians should be cautious in treating patients with a history of hypertrophic scarring or keloid formation3. Nevertheless, in the study of Taylor et al,102 none of the 150 patients developed a keloid.
The most important aspect of facial volumization in male patients of color is intimate knowledge of the structural differences between them and Caucasians and honoring the aesthetic ideals that they are aspiring toward. Most often than not, individuals of ethnic backgrounds are not seeking a “Westernized” version but rather a “rejuvenated” version of themselves (Fig. 10.2). For example, African American women usually experience fine lines, and loss of volume below the vermillion border, of the upper lip, and thus seek augmentation of the upper lip area.104 This is achieved by superiorly rolling the lip using low-viscosity HA fillers such as Belotero (Merz Aesthetics, Raleigh, North Caroline, United States) or Restylane silk (Galderma, Fort Worth, Texas, United States). Moreover, the collagen content and collagen-production capacity of African Americans is higher than that of Caucasians, thus treating with soft-tissue fillers that have biostimulatory properties such as PLLA (Galderma) and CaHa (Radiesse; Merz Aesthetics) can be more effective in this population, and as a result they will require fewer treatments than their white counterparts.
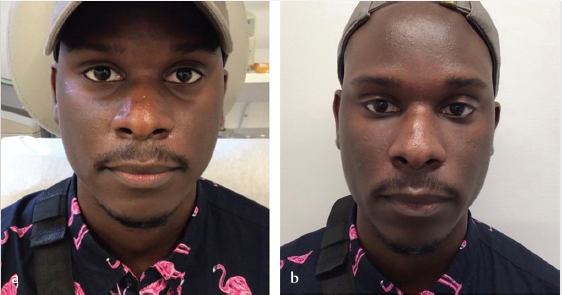
Fig. 10.2 A 37-year-old African American man before (a) and two weeks after (b) volumization with 2-mL hyaluronic acid filler in the midface.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








