Fig. 15.1
Despite technical advances, vascular insufficiency, shape and positioning of the umbilicus, and scar location are still major problems after abdominoplasty. (Left) Skin, fat, and umbilical stalk necrosis after conventional lipoabdominoplasty as was observed 2 weeks after surgery. (Center) Poor result and displeased patient after conventional abdominoplasty, she complains of high scar and umbilicus that is wide and low. (Right) Stenotic umbilicus after abdominoplasty with associated problems as irritation, infection, poor hygiene, and bad odor

Fig. 15.2
“Dome effect” after vertical plicature through an epigastric tunnel during conventional lipoabdominoplasty. (Left) Outline of vertical plicature during lipoabdominoplasty, most of the flap is attached to underlying muscles and vessels. During plicature, tissues are brought to midline. (Center) Poor result after lipoabdominoplasty, skin epigastric redundancy is observed, despite liposuction. Tissues are brought together in midline by the underlying plicature. (Right) Same patient demonstrates her desire to attain a flat epigastrium doing bimanual skin traction
Therefore, the biggest surgical challenge despite abdominoplasty evolution is vascular flap safety, to attain a flat abdominal surface without redundancies especially in epigastrium, to locate the transverse scar sufficiently in low position to hide it within the underwear or bathing suit limits, and to obtain an umbilicus of good appearance and location.
Continuing in the evolutionary way to solve the historical challenges of abdominoplasty, several modifications to the technique have been made since 2005, grouped under the acronym TULUA [4]:
1.
Transverse abdominal wall plication, instead of vertical
2.
Abolition of flap detachment above the navel, rather than wide dissection or undermining restricted to a tunnel
3.
Liposuction without restrictions, rather than limited or conditioned liposuction
4.
Amputation of the original belly button followed by neoumbilicoplasty with a skin graft, rather than exteriorization umbilicoplasty
5.
Adequate and low-level location of the transverse scar in all cases, instead of random location or where the tension of the flap permitted (Table 15.1) [5, 6]
Table 15.1
TULUA abdominoplasty modifications compared with lipoabdominoplasty and conventional abdominoplasty
Lipoabdominoplasty and conventional abdominoplasty | Modifications in TULUA abdominoplasty | |
|---|---|---|
Vertical plicature | T | Transverse (plicature) |
Wide dissection | U | Undermining halted at umbilicus (no epigastric flap detachment) |
Without liposuction or limited (danger zones) | L | Liposuction (without restrictions) |
Umbilicoplasty by stump exteriorization | U | Umbilicoplasty with a skin graft |
Abdominoplasty with no very low scar location due to flap tension | A | Abdominoplasty with low transverse scar localization |
This chapter is a description of the paradigm shift that TULUA modifications do to the conventional philosophy in abdominoplasty. This different way of thinking may be an alternative for those who are involved in making plastic surgery safer and more reliable.
15.2 Surgical Technique
15.2.1 Patient Selection
TULUA abdominoplasty can be applied to any patient; nevertheless as in the conventional surgery, it has relative contraindications in smokers, obese, and in the presence of comorbidities. It definitely cannot be used if there is significant diastasis recti above the navel and hernias or epigastric eventrations, which have been determined by physical examination or imaging. However, some cases of umbilical hernias or eventrations in the lower abdomen could be treated simultaneously with this technique.
TULUA is especially indicated in patients in whom flap detachment of the epigastrium is considered risky or inappropriate due to vascularity concern as well as in obese, smokers and in cases of previous liposuction. Obese patients in whom it is not possible or there is no indication of bariatric surgery are particularly benefited from this type of surgery, without having to deal with extensive dissection to reposition the umbilical stalk which is elongated and is hard to accommodate in some cases. For the same reasons, the technique has special advantages for massive weight loss patients. The modifications would have application when there is redundancy of skin and epigastric fat, where accumulation of tissue in the midline of the upper abdomen with vertical plication is anticipated. Probably some cases of vertical excess of skin, in whom a “fleur-de-lis” resection is considered to leave a final anchor-shaped scar, can be beneficiaries of TULUA, avoiding perhaps the vertical scar component (Fig. 15.3). In conclusion, TULUA technique can be applied to any patient who has no significant diastasis or hernia in the epigastrium, most of patients in whom has been used have been selected in an intuitive manner, in cases where is deemed inconvenient or unsafe a wide flap dissection (Table 15.2).
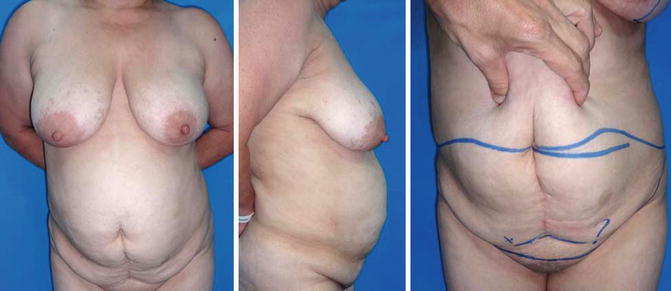
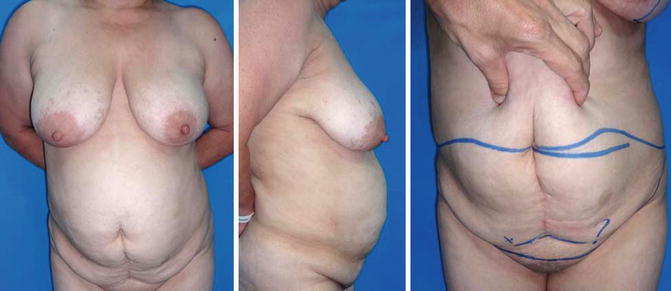
Fig. 15.3
Patient selection for TULUA abdominoplasty. (Left) 45-year-old obese patient with BMI 32, a passive smoker, with skin and fat redundancy at the epigastrium level, intuitively judged as a good candidate for TULUA. (Center) Abdominal bulge observed in lateral view, epigastric hernia, and significant diastasis were ruled out by physical exam. (Right) Digital pinch test demonstrates fat deposits to be removed with unrestricted liposuction of the epigastrium. Skin excess will be evenly distributed with the downward traction of the flap, no skin excess in epigastric midline will be observed after surgery
Table 15.2
Indications of TULUA abdominoplasty in 42 patients
Primary cases | 32 |
Revisional cases | 10 |
Obesity | 22 |
Smokers | 3 |
Epigastric skin and fat redundancy | 10 |
Once the patient has been selected and other surgical options discussed, informed consent for surgery is mandatory in which sufficient clarity about modifications to the technique is emphasized.
15.2.2 Surgical Markings
With the patient standing, demarcation is similar to conventional abdominoplasty, taking care to place the transverse incision as low enough at the time of surgical wound closure about 5–7 cm above the anterior vulvar commissure, and the incision should be planned sufficiently to avoid lateral dog ears.
In no case, the preexisting lower abdominal crease is used to plan the incision; subsequently, this leads to high location of the scar. By contrast during demarcation, the patient is asked to pull up firmly and symmetrically with both hands the skin and fat from the hypogastrium, noticing a shift of the mons veneris and the vulva to a higher and anterior placement; in this situation of transient traction, a midline mark point is placed 5–7 cm above the anterior vulvar commissure, bimanual traction is then released, and the outline proceeds all the way of the transverse incision starting from the central point to the most lateral end, frequently exceeding the anterior iliac spines. An ellipse is completed drawing a joining line between the lateral ends with the navel; the upper and lower outlines of the ellipse should be approximately of the same length to facilitate the closure without dog ears, rotation cones, or lateral deformities (Fig. 15.4).


Fig. 15.4
Typical presurgical markings for TULUA. (Left): Skin redundancy and fat excess at the epigastrium were the main indications of TULUA. (Right) Bimanual upward traction allows exact placement of the scar 5–7 cm above the anterior vulvar commissure. Lateral prolongations are necessary to avoid dog ears
15.2.3 Surgical Procedure
Under general anesthesia, infiltration with saline and adrenaline 1: 500,000 is completed to achieve tumescence in the anterior abdomen and all areas in which there will be liposuction that usually involve the back, flanks, and medial thighs. Average infiltration of the abdomen is 2000 mL, which is complemented to 3000–8000 mL in all additional operative areas.
Through four ports of 5 mm in hypogastrium, one in the navel and two in the inframammary crease, full deep and superficial liposuction is carried out, above the navel, abdominal flanks, and mons veneris using cannulas of 5 mm. Liposuction is done without any restriction as recommended in other techniques, leaving the flap thin and uniform, about 2–3 cm in thickness with multiple crisscrossed cannula tunnels. Additional ports are used, according to the surgical plan, to complete liposuction in the back and remaining areas under treatment; liposuction of the hypogastrium is not considered necessary because it will be resected en bloc afterward (Fig. 15.5).
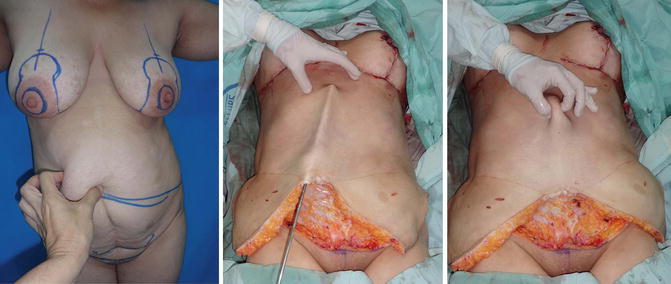
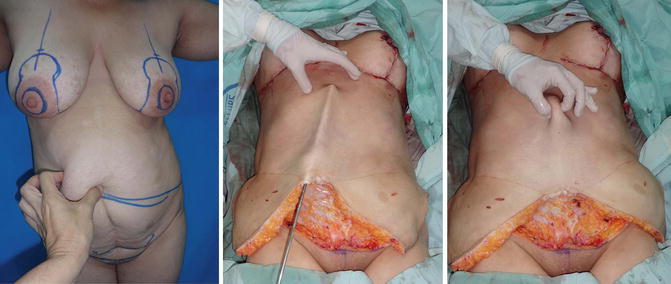
Fig. 15.5
Full unrestricted tumescent liposuction is permitted during TULUA abdominoplasty. (Left) Obese patient with a thick epigastric flap as demonstrated by digital pinch maneuver. (Center) No epigastric flap elevation was performed. After tumescence ample liposuction was accomplished with a 5 mm cannula. (Right) Digital pinch test demonstrates flap thinning and skin mobility with liposuction
A bistoury skin incision is performed on the delineated transverse line, down to the subcutaneous fat. With an electrocautery, dissection in a surgical plane immediately above the muscular aponeurosis is carried out. The hypogastric flap is detached up as far as the umbilicus, halting at its level, creating a limit of upper dissection that unites the iliac spines with the navel in the midline. In no case, direct flap elevation must progress above the navel. It is recommended to leave a little fat over the pubic bone doing an oblique or step cutting after the initial skin incision, forming a subcutaneous triangle about 6 by 4 cm where the thinner part of the supraumbilical flap will be accommodated (Fig. 15.6).


Fig. 15.6
During TULUA procedure, the umbilicus is amputated. Direct dissection of the hypogastric flap is halted at umbilical level. (Left) Black arrow demonstrates wall defect of the amputated umbilicus. Direct flap dissection is stopped at this level. Yellow dotted lines on the suprapubic area delineate a beveled dissection in order to preserve some tissues to fill the fat defect observed around the umbilicus in the flap border (see delineated triangular area with additional yellow dotted line). (Center) A 30 by 11 cm ellipse is outlined on the anterior hypogastrium. (Right) Liposuction tunnels and transverse plicature allow easy downward flap sliding to permit a tension-free closure
After complete dissection of the hypogastrium, a horizontal ellipse is drawn with a surgical marker on the anterior musculature of the abdomen from the iliac spine to the other, passing through the umbilicus and pubis. To determine if the size of the drawn ellipse is correct for the plication, an active maneuver is performed sinking the wall with four fingertips extended in the center of the elliptical mark, to observe how the top and bottom lines come together to almost touching; if there is some lateral redundancy over the oblique muscles on the iliac crest, the plicature could extend laterally about 4 cm more on each side.
With the patient under muscle relaxation and the operating table in a position of moderate flexion, transverse plication of the anterior wall of the abdomen is carried down joining the edges of the drawn ellipse, with interrupted 0 polypropylene stitches with inverted knots, which are reinforced by running suture of the same suture type (Fig. 15.7).
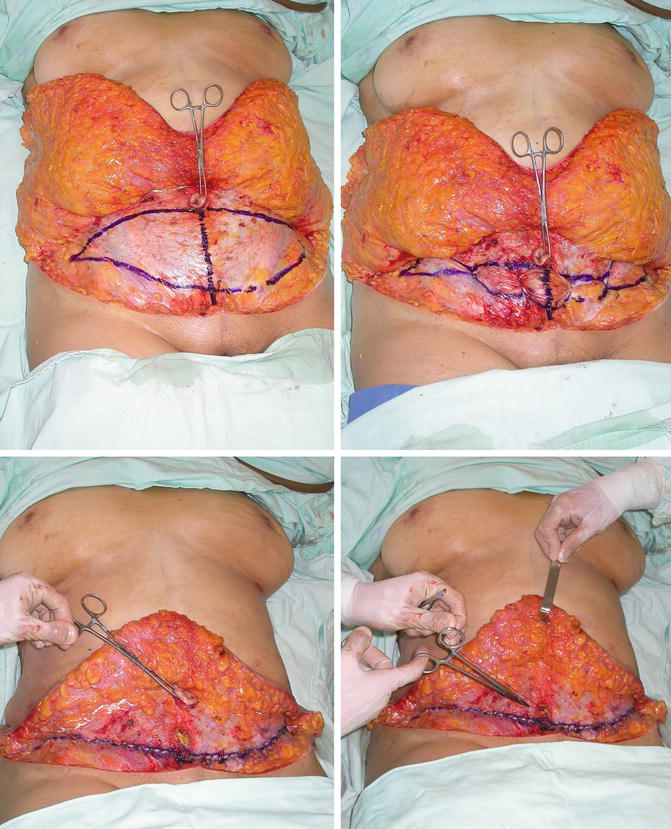
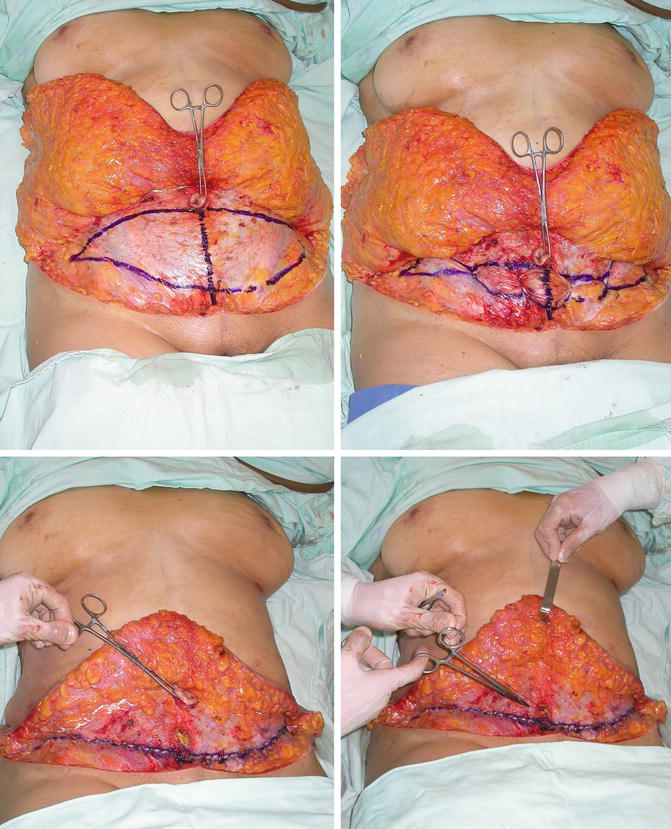
Fig. 15.7
Transverse plicature and original umbilicus amputation are major distinctive steps during TULUA abdominoplasty. (Top left) A hypogastric ellipse 34 by 12 cm is outlined. Skin and fat from the lower abdomen have been detached to the umbilicus; a midline partition of the detached flap facilitates upward folding over the epigastrium. (Top right) Individual sutures of 0 polypropylene are placed to start the aponeurotic folding; full muscle relaxation under general anesthesia and mild flexed position of the operating table facilitate this step. (Bottom left) 1300 g of skin and fat has been removed from the hypogastrium, an Allis clamp is holding the amputated umbilicus, and a second uninterrupted layer of 0 polypropylene completes the transverse plication. (Bottom right) Umbilicus defect must be closed with additional sutures
This plication reaches 30 per 10 cm, and it can be extended while it is made if, laxity or on the contrary, excessive tension is observed. This surgically created fold produces umbilical descent reaching the pubis in some cases. The navel is then amputated, and its abdominal wall opening is closed with 0 polypropylene stitches.
The fat and skin previously elevated of the hypogastrium are resected, which in all cases is a similar block of tissues than is resected in conventional surgery. The wound is closed by planes emphasizing to avoid dog ears using additional liposuction and lateral prolongation of the incision as necessary. This wound closure is much easier and under less tension than in conventional abdominoplasties as tension on the suture line is not exerted directly on the skin, but it is mitigated by the pulling effect of the aponeurosis and the accompanying downward displacement of all tissues during the transverse plication.
The wound closure is done with 2-0 polyglactin stitches at the subcutaneous planes, superficial aponeurosis, and dermis. The skin is sutured with 3-0 poliglecaprone or 3-0 polypropylene intradermal continuous suture. Wound dead space is reduced performing this careful closure, and the flap gently reaches almost without tension to the bottom edge of the wound (Fig. 15.8).


Fig. 15.8
After transverse plicature and full liposuction, the tension-free closure is facilitated. (Left) Transverse plicature has been completed in two layers, original umbilicus has been sectioned at its base, and the resulting defect closed; no flap elevation has been performed above the umbilicus. The hypogastric flap to be resected is folded over. (Center) Gentle traction of the abdominal flap demonstrates how easy the closure is. Note the uniform distribution of the tissues on the new abdominal wall; no distortions and irregularities due to residual adherences to deep tissues (“dome effect”) are observed. Epigastric skin excess is evenly distributed. (Right) After wound closure in layers, a midline has been traced, and a new umbilicus position determined 9 cm above the transverse incision (H: 9); note the low positioning of the transverse scar 5.5 cm (V: 5.5) from the anterior vulvar commissure (V/H ratio: 5.5/9 = 0.6)
A closed suction drainage is left in place for 7 days through two incisions at mons veneris.In secondary cases, the subcutaneous tissues and superficial fascia of the upper border of the incision, are set with slowly absorbable sutures to firm pubic spots and iliac spines to prevent, or correct the superior migration of the scar.
At this moment in surgery, there have been significant changes in the anterior abdominal wall, which must be seen flat, without irregularities, with tense aponeurosis due to transverse plication and the skin without redundancies or abnormal accumulations (dome effect), as sometimes seen in cases of abdominoplasties with plication in the midline.
On the abdominal skin now sutured, a vertical midline is drawn from the xiphoid to the vulva. The measured distance from the surgical wound to the top part of the vulvar commissure must continue being 5–7 cm (distance V) as was planned, this distance is multiplied by 1.5–2, and the measurement is translated in the midline above the abdominal incision to help to choose the best position of the new umbilicus 7.5–14 cm (distance H). Once determined the ideal umbilical position, an inverted U incision, is made 1.5 cm in diameter; fat trimming with scissors is performed down its periphery to the muscular fascia and linea alba, creating a depression of 2.5 cm.
For best viewing of the linea alba, curettage of fat can be performed with a Yankauer cannula with its olive tip temporarily removed by hand unscrew. Sloped walls of the umbilicus are formed joining the dermis of the inverted U incision to the abdominal aponeurosis, with six to eight polyglactin 2-0 sutures. Senn-Miller retractors are used for easier setting of sutures in such a small space; traction from the bottom of the wound with a temporary suture can also help during the process; stitches are placed all first, leaving them unknotted and repaired with mosquito forceps, to be all tied to the end, resulting in a closure with lost inverted knots between the fascia and skin.
A full-thickness skin graft, triangular shaped of 1.5 cm, perfectly defatted, is harvested from the hypogastrium-resected specimen, to be attached to the abdominal wall with three sutures of 3-0 plain catgut, to create the bottom of the neoumbilicus. The skin graft must be in intimate contact for its dermal side with the aponeurosis of the abdominal midline. Additional sutures can be placed if necessary. Graft must be flat; in no case it is tubular, and the recipient area is never a fatty tissue. An antibiotic ointment dressing is used forming a ball of 1.5 cm to help give form to the new navel (Figs. 15.9 and 15.10).

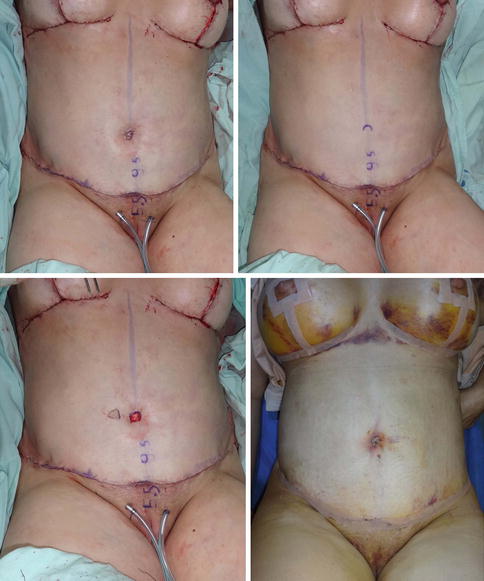

Fig. 15.9
Neoumbilicoplasty with a skin graft. (Left) After determining the new umbilicus position, an inverted U incision is performed. Perimetric fat trimming creates a periumbilical depression; borders of the U incision are sutured with 2-0 polyglactin interrupted sutures to the abdominal fascia, forming a central hole with surrounding depression and beveled walls. (Center) A small 1 cm full-thickness skin graft is firmly sewed with 3-0 plain catgut on the linea alba of the abdominal wall to create the bottom of the new navel. (Right) Late result in the same patient, a relatively high umbilicus is observed with a V/H ratio of 0.46; however, this result demonstrates the total freedom in umbilicus positioning. Careful umbilicus positioning with a better V/H ratio is important to achieve constantly good results, as was performed in subsequent cases
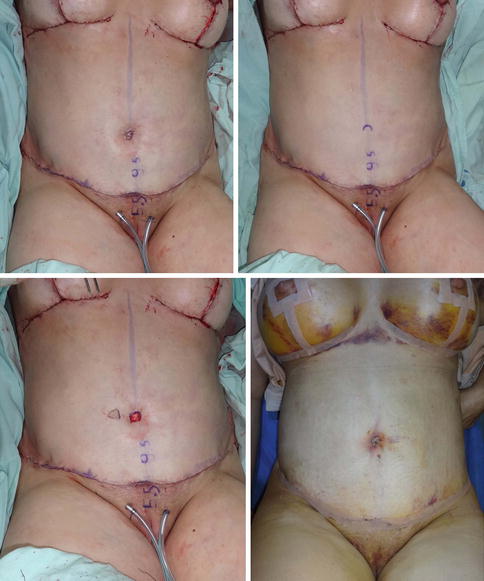
Fig. 15.10
Graft take after neoumbilicoplasty in TULUA. (Top row and bottom left) Successive steps for new umbilicus creation. (Bottom right) In the same patient, graft take at day 7 after surgery, no signs of flap ischemia or wound dehiscence are noted at the transverse incision
After the surgery is completed, a postsurgical elastic garment is worn to produce moderately elastic compression of the abdomen and operated areas. The patient is transferred to standard postoperative room to be discharged the next day with home care of wound and drain. The drain is usually removed after a week regardless of their production; in the few cases that seromas are seen, they are drained aseptically by needle and syringe puncture during postoperative consultations once or twice a week until complete remission of the collection (Table 15.3).
Table 15.3
Technical details in TULUA abdominoplasty
Patient selection | Obese, massive weight loss, postbariatric, epigastric redundancy, smoking (active, passive), revisional cases (any patient according to surgeon’s “intuitive” criteria) |
Surgical markings | Strong bimanual traction, central point 5–7 cm above the anterior vulvar commissure |
Liposuction | Tumescent, without restriction to the upper anterior abdomen, midline, and flanks |
Excision of abdominal panniculus in hypogastrium | En bloc resection, no liposuction, no Scarpa’s fascia preservation |
Plicature | Transverse, from navel to pubis, or less if excessive tightness does not allow. Between anterior iliac spines or wider if necessary |
Wound closure | No tension. Scarpa’s, subcutaneous fat and dermis closure |
Neoumbilicoplasty | Small skin graft, only to create the bottom of navel 1.5 cm. inverted U-shaped incision, U borders of skin attached to fascia with sutures |
Drains | Closed for 1 week |
15.3 Prior Publication
In a previous publication by the author, data from 42 women were reported operated with TULUA technique from January 2005 until June 2011. Although it was a case report series, results were objectively measured for greater accuracy [7]. Demographics of the series, follow-up, and operative data are as follows: age 22–64 years (average 47 ± 12). The main consultation complaints were esthetic, but in one case, it was after weight loss and one more as hygienic panniculectomy. In ten patients, the primary indication was epigastric excess of skin and fat. Average body mass index (BMI) was 30 ± 3.6 (range 22–38). Twenty-two of 42 patients were obese with a BMI >30.
Most of the patients had during surgery liposuction of additional areas without measurement of extracted fat for the isolated abdominal area. The total amount of the aspirate was quantified without separation of the liquid components of fat and blood, being on average 4255 mL (range 1000–7000 mL).
The resected ellipse of skin and fat from the hypogastrium was in average 1375 g with variations from 540 g up to 5000 g (Table 15.4). The size of the transverse elliptical plication was 24–34 cm wide (average 30.7 ± 2.3) and 6–13 cm high (average 9.8 ± 2.1). The area of the plication calculated by the formula of the area of an ellipse (π × r1 × r2) was on average 236 ± 55 cm2 with 118 cm2 minimum and maximum of 337 cm2




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







