Procedure 90 Total Wrist Arthroplasty
Indications
 Destructive and painful wrist conditions resulting from rheumatoid arthritis (RA), osteoarthritis (OA), or trauma
Destructive and painful wrist conditions resulting from rheumatoid arthritis (RA), osteoarthritis (OA), or trauma
 The procedure is contraindicated in patients with the following conditions:
The procedure is contraindicated in patients with the following conditions:
Examination/Imaging
Clinical Examination
 One must evaluate active and passive wrist range of motion to determine any presence of carpal subluxation or dislocation and distal radioulnar (DRU) joint stability.
One must evaluate active and passive wrist range of motion to determine any presence of carpal subluxation or dislocation and distal radioulnar (DRU) joint stability.
 Additionally, the integrity of the flexor and extensor tendons of the wrist and hand should be assessed.
Additionally, the integrity of the flexor and extensor tendons of the wrist and hand should be assessed.
 One must perform a detailed history of the patient’s functional demands, activities, occupation, hobbies, and home circumstances. Patients should be given a trial of splint immobilization, and arthroplasty should be considered for those who find that period of immobilization intolerable.
One must perform a detailed history of the patient’s functional demands, activities, occupation, hobbies, and home circumstances. Patients should be given a trial of splint immobilization, and arthroplasty should be considered for those who find that period of immobilization intolerable.
Imaging
 Posteroanterior, oblique, and lateral radiographs of the wrist are essential to determine extent of wrist destruction. Conditions such as scapholunate advanced collapse (SLAC) and scaphoid nonunion advanced collapse (SNAC) should be noted.
Posteroanterior, oblique, and lateral radiographs of the wrist are essential to determine extent of wrist destruction. Conditions such as scapholunate advanced collapse (SLAC) and scaphoid nonunion advanced collapse (SNAC) should be noted.
 Additional views of the wrist or computed tomography can be obtained to further evaluate arthritis or to assess less obvious intercarpal arthrosis.
Additional views of the wrist or computed tomography can be obtained to further evaluate arthritis or to assess less obvious intercarpal arthrosis.
 Wrist arthroscopy may determine whether limited wrist fusion is preferable. Patients with a preserved radiocarpal joint should be considered for motion-sparing wrist procedures such as four-corner bone fusion or proximal row carpectomy. Rheumatoid patients with radiocarpal arthritis but a preserved midcarpal joint may be eligible for radiolunate or radioscapholunate fusion to maintain midcarpal motion.
Wrist arthroscopy may determine whether limited wrist fusion is preferable. Patients with a preserved radiocarpal joint should be considered for motion-sparing wrist procedures such as four-corner bone fusion or proximal row carpectomy. Rheumatoid patients with radiocarpal arthritis but a preserved midcarpal joint may be eligible for radiolunate or radioscapholunate fusion to maintain midcarpal motion.
Surgical Anatomy
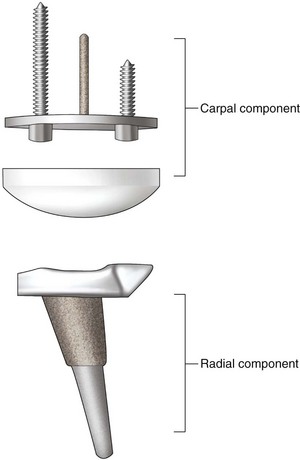
 The implant described in this chapter is the Universal II implant design, which is the most popular total wrist arthroplasty implant used in the United States. Other implant designs are available, but comparative or long-term studies are not presented to determine which implant type is most durable and has the lowest complication rate. The implant design consists of two components. The carpal component is fixated with two screws (Fig. 90-1).
The implant described in this chapter is the Universal II implant design, which is the most popular total wrist arthroplasty implant used in the United States. Other implant designs are available, but comparative or long-term studies are not presented to determine which implant type is most durable and has the lowest complication rate. The implant design consists of two components. The carpal component is fixated with two screws (Fig. 90-1).
 The radial component has an articular inclination of 15 degrees to simulate the anatomy of the distal radius.
The radial component has an articular inclination of 15 degrees to simulate the anatomy of the distal radius.
 Distal and proximal stems are porous coated, which has the theoretical advantage of allowing osseointegration of the components.
Distal and proximal stems are porous coated, which has the theoretical advantage of allowing osseointegration of the components.
 The size of the implant placed can be estimated preoperatively from the wrist radiograph.
The size of the implant placed can be estimated preoperatively from the wrist radiograph.
Exposures
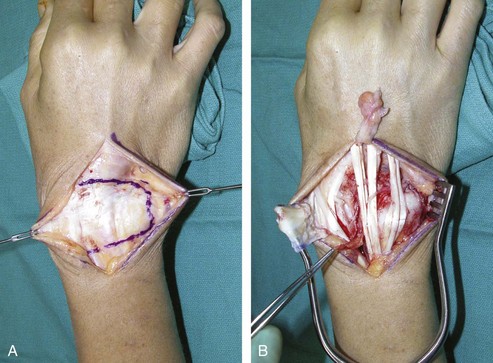
 An 8-cm incision is made on the dorsal wrist, centered on the axis of the long finger metacarpal (Fig. 90-2).
An 8-cm incision is made on the dorsal wrist, centered on the axis of the long finger metacarpal (Fig. 90-2).
 Radial and ulnar skin flaps are elevated, and the extensor retinaculum is visualized.
Radial and ulnar skin flaps are elevated, and the extensor retinaculum is visualized.
 The entire extensor retinaculum is elevated from the sixth dorsal compartment all the way to the radial attachment over the first compartment. The septa between the compartments are taken down to create a continuous flap of extensor retinaculum. The elevation of the extensor retinaculum stops between the first and second compartments (Fig. 90-3).
The entire extensor retinaculum is elevated from the sixth dorsal compartment all the way to the radial attachment over the first compartment. The septa between the compartments are taken down to create a continuous flap of extensor retinaculum. The elevation of the extensor retinaculum stops between the first and second compartments (Fig. 90-3).
 The extensor tendons are then retracted to expose the wrist.
The extensor tendons are then retracted to expose the wrist.
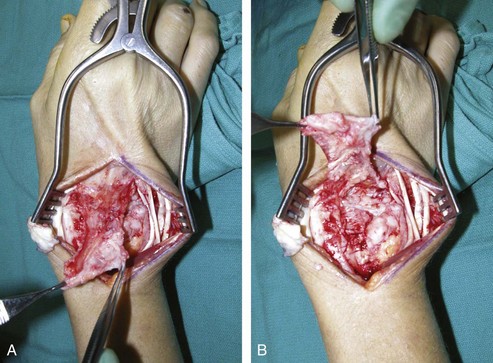
 The wrist capsule is elevated subperiosteally proximal to the radiocarpal joint as a rectangular, distally base flap (Fig. 90-4A and B). The purpose of the wrist capsular flap is to cover and to provide stout capsular support for the implant.
The wrist capsule is elevated subperiosteally proximal to the radiocarpal joint as a rectangular, distally base flap (Fig. 90-4A and B). The purpose of the wrist capsular flap is to cover and to provide stout capsular support for the implant.
Pearls
If there is arthritic change involving the DRU joint, a Darrach procedure is performed by resecting the distal ulna at a 45-degree oblique apex-ulnar angle. RA patients often have DRU disease, and distal ulna excision is performed to alleviate future problems. For OA patients with only radiocarpal disease, the radioulnar joint can be preserved.
The head of the resected ulna should be saved for bone graft.
The ECRB, and preferably the ECRL tendon as well, should be intact or otherwise reconstructible.
A segment of the posterior interosseous nerve can be excised just proximal to the radiocarpal joint.
Procedure
Step 1
 The wrist is flexed to have an end-on view of the radius articular surface. A bone awl is placed 5 mm below the dorsal articular surface of the radius just slightly radial to the Lister tubercle (Fig. 90-5).
The wrist is flexed to have an end-on view of the radius articular surface. A bone awl is placed 5 mm below the dorsal articular surface of the radius just slightly radial to the Lister tubercle (Fig. 90-5).
 The radial alignment guide is inserted into the cavity created by the awl, and fluoroscopy is used to confirm that the guide rod is centered in the radius, both in the anteroposterior and lateral planes (Fig. 90-6).
The radial alignment guide is inserted into the cavity created by the awl, and fluoroscopy is used to confirm that the guide rod is centered in the radius, both in the anteroposterior and lateral planes (Fig. 90-6).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree