Chapter 9 Incision Approaches
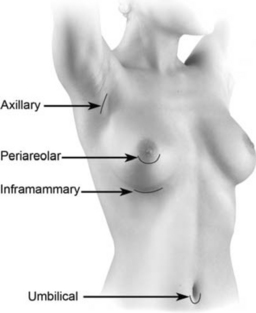
Four incision approaches are currently used for primary breast augmentation: inframammary, axillary, periareolar, and umbilical (Figure 9-1). This chapter provides an overview and comparison of incision approaches, and Chapters 11, 12, and 13 address the inframammary, axillary, and periareolar approaches in detail.
Issues and Selection Criteria for Incision Approach
Patients who have an optimal result from breast augmentation rarely express any concern whatever about the location of their scar, positively or negatively. Absent gross scar hypertrophy or scar malposition, educated patients understand that a scar is a necessary tradeoff of augmentation, that the location of the scar is not as important as the quality of the result, and that few normal observers of a beautiful breast pay much attention to any scar (just as few observers would pay much attention to a stretch mark). Incision location is much more a preoperative concern than a postoperative concern, provided the surgeon educates the patient and applies basic principles to optimize scar quality. The most important of principles to optimize scar quality in every case, regardless of skin type or other considerations, include: (1) adequate incision length to minimize trauma to skin edges for access and implant insertion, (2) avoiding trauma to skin edges during the procedure, (3) optimal incision location to minimize tension and stretch on the incision, and (4) optimal incision closure techniques that minimize tension on the skin while also minimizing the amount of suture left in the wound to stimulate inflammation.
Incision Location Choice in the Decision Process
Incision location is the fifth priority decision of the High Five™ decision process algorithm for primary breast augmentation.2 Decisions to choose pocket location, implant volume (weight), implant type, and location of the inframammary fold decisions precede selection of incision location. Prioritizing incision location choice above any of the other considerations potentially compromises the outcome, especially the long-term outcome, because the incision location decision does not directly impact the quality of the patient’s tissues long-term or the position of the breast on the chest.
In the United States, informed consent law requires that patients make choices regarding their medical care. Surgeons can provide information and assist in the decision process, but patients ultimately must choose the options for their care that they determine are best. Surgeons can easily influence a patient’s choice of incision location through the content of information they provide the patient, but surgeons are legally responsible for providing the patient valid information about all options during the informed consent process and documenting that the patient understands the options. Informed consent law requires that the patient make the final decision of incision location.
Popular Myths Regarding Incision Location
The Inframammary Incision Location—Advantages and Tradeoffs
Compared to all other incision approaches, the inframammary approach causes the least trauma to adjacent tissues for pocket access and implant insertion. All areas of the implant pocket are directly visible and accessible through this approach, and surgeons can precisely complete pocket dissection in all pocket locations and place all types of breast implant via this approach. The inframammary approach requires no special instrumentation, and is the most efficient of all approaches with respect to minimizing operative times, thereby minimizing drug dosages and optimizing patient recovery.1 In the author’s published study detailing techniques that deliver predictable 24 hour recovery, comparable recovery was achieved via inframammary, periareolar, and axillary approaches, but operative times were longer for periareolar and axillary approaches compared to the inframammary approach.1
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 The inframammary incision approach is the most widely used incision approach in breast augmentation. Based on published data and logic, the inframammary approach is the incision approach to which surgeons should objectively compare all other incision approaches. The inframammary incision approach provides a level of direct vision and surgical control that is unmatched by other incision locations, and enables surgeons to achieve greater control over a greater number of surgical variables that affect outcomes. The most important of these variables are the degree of tissue trauma and bleeding that occur during the operation, the degree of precision during pocket dissection, and the ease with which the surgeon can introduce the implant without damaging the device. No incision approach surpasses the inframammary approach with respect to these three important considerations.
The inframammary incision approach is the most widely used incision approach in breast augmentation. Based on published data and logic, the inframammary approach is the incision approach to which surgeons should objectively compare all other incision approaches. The inframammary incision approach provides a level of direct vision and surgical control that is unmatched by other incision locations, and enables surgeons to achieve greater control over a greater number of surgical variables that affect outcomes. The most important of these variables are the degree of tissue trauma and bleeding that occur during the operation, the degree of precision during pocket dissection, and the ease with which the surgeon can introduce the implant without damaging the device. No incision approach surpasses the inframammary approach with respect to these three important considerations.




