Procedure 88 Four-Corner Fusion Using a Circular Plate
![]() See Video 66: 4-Corner Fusion with a Circular Plate
See Video 66: 4-Corner Fusion with a Circular Plate
Examination/Imaging
Clinical Examination
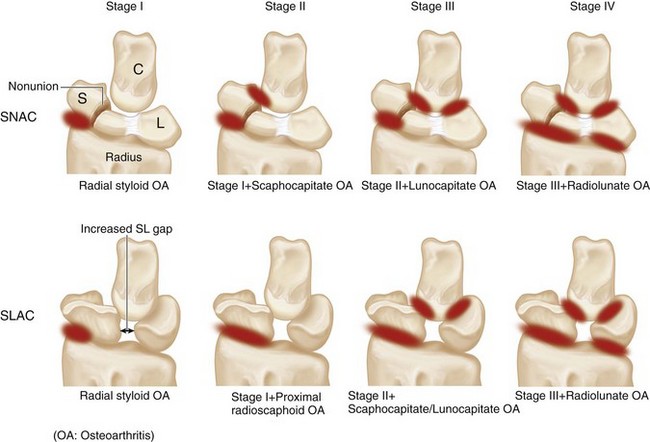
 A sequential progression of arthritic changes has been described for scaphoid nonunion and static scapholunate instability. They are called the scaphoid nonunion advanced collapse (SNAC) and scapholunate advanced collapse (SLAC), respectively (Fig. 88-1).
A sequential progression of arthritic changes has been described for scaphoid nonunion and static scapholunate instability. They are called the scaphoid nonunion advanced collapse (SNAC) and scapholunate advanced collapse (SLAC), respectively (Fig. 88-1).
 A four-corner fusion involves removal of the scaphoid (only the distal scaphoid may be removed in SNAC) and fusion of the lunate, triquetrum, capitate, and hamate. The other option is a proximal row carpectomy (PRC) that involves removal of the scaphoid, lunate, and triquetrum and allows the capitate to articulate in the lunate fossa of the radius.
A four-corner fusion involves removal of the scaphoid (only the distal scaphoid may be removed in SNAC) and fusion of the lunate, triquetrum, capitate, and hamate. The other option is a proximal row carpectomy (PRC) that involves removal of the scaphoid, lunate, and triquetrum and allows the capitate to articulate in the lunate fossa of the radius.
 A four-corner fusion is the preferred option in stage III SNAC/SLAC because the capitolunate joint is arthritic and a PRC will result in an arthritic capitate articulating with the lunate fossa.
A four-corner fusion is the preferred option in stage III SNAC/SLAC because the capitolunate joint is arthritic and a PRC will result in an arthritic capitate articulating with the lunate fossa.
 In stage II SNAC/SLAC, a PRC or a four-corner fusion may be done. A PRC is simpler and does not rely on fusion of small carpal bones. A four-corner fusion maintains carpal height and provides better hand strength compared with PRC.
In stage II SNAC/SLAC, a PRC or a four-corner fusion may be done. A PRC is simpler and does not rely on fusion of small carpal bones. A four-corner fusion maintains carpal height and provides better hand strength compared with PRC.
 A diagnosis of SNAC or SLAC wrist is often made in patients who seek medical advice for other conditions of the wrist. They are usually minimally symptomatic or asymptomatic, tend to be older, and engage in less physically demanding tasks. This group of patients should be managed conservatively with activity modification, intermittent splintage, and nonsteroidal analgesics. Surgery should be reserved for patients who fail conservative measures or in younger symptomatic patients in whom further progression of arthritis can be prevented.
A diagnosis of SNAC or SLAC wrist is often made in patients who seek medical advice for other conditions of the wrist. They are usually minimally symptomatic or asymptomatic, tend to be older, and engage in less physically demanding tasks. This group of patients should be managed conservatively with activity modification, intermittent splintage, and nonsteroidal analgesics. Surgery should be reserved for patients who fail conservative measures or in younger symptomatic patients in whom further progression of arthritis can be prevented.
Imaging
 Standard wrist posteroanterior and lateral views are usually sufficient in SNAC/SLAC wrists. One should be able to determine whether there is arthritis involving the capitate (PRC cannot be done) or arthritis involving the lunate fossa of the radius (both PRC and four-corner fusion cannot be done). If the radiograph shows ulnar translocation of the carpus, it means that the palmar radiocarpal ligaments, especially the radioscaphocapitate, are lax, and a PRC cannot be done.
Standard wrist posteroanterior and lateral views are usually sufficient in SNAC/SLAC wrists. One should be able to determine whether there is arthritis involving the capitate (PRC cannot be done) or arthritis involving the lunate fossa of the radius (both PRC and four-corner fusion cannot be done). If the radiograph shows ulnar translocation of the carpus, it means that the palmar radiocarpal ligaments, especially the radioscaphocapitate, are lax, and a PRC cannot be done.
 If the condition of these joints cannot be clearly assessed by a radiograph, a computed tomography scan or a wrist arthroscopy should be considered.
If the condition of these joints cannot be clearly assessed by a radiograph, a computed tomography scan or a wrist arthroscopy should be considered.
Surgical Anatomy
 The distal radius has two articular fossae for the scaphoid and lunate. The scaphoid fossa is shaped like a spoon and narrows as it approaches the radial styloid. This results in incongruency between the scaphoid and the scaphoid fossa during positional changes and results in uneven loading of scaphoid fossa, making degenerative changes of the radioscaphoid joint common. On the other hand, the lunate fossa is spherical and remains congruently loaded in all positions of the lunate, making the radiolunate joint highly resistant to degenerative changes.
The distal radius has two articular fossae for the scaphoid and lunate. The scaphoid fossa is shaped like a spoon and narrows as it approaches the radial styloid. This results in incongruency between the scaphoid and the scaphoid fossa during positional changes and results in uneven loading of scaphoid fossa, making degenerative changes of the radioscaphoid joint common. On the other hand, the lunate fossa is spherical and remains congruently loaded in all positions of the lunate, making the radiolunate joint highly resistant to degenerative changes.
Exposures
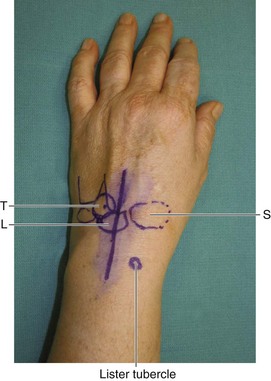
 A 6-cm dorsal longitudinal incision centered over the radiocarpal joint in line with the long finger metacarpal is made (Fig. 88-2). Sharp dissection is carried down to the extensor retinaculum. Skin and subcutaneous tissue flaps are raised on both sides. The third dorsal compartment is identified and opened along its entire length. The extensor pollicis longus (EPL) tendon is left in its sheath and not transposed. One must know the location of the EPL when incising the wrist capsule proximally. The wrist capsule is opened longitudinally and dissection performed to elevate the second and fourth compartments such that the second and fourth compartment tendons are maintained within the compartment. This exposes the scaphoid, lunate, triquetrum, capitate, and hamate.
A 6-cm dorsal longitudinal incision centered over the radiocarpal joint in line with the long finger metacarpal is made (Fig. 88-2). Sharp dissection is carried down to the extensor retinaculum. Skin and subcutaneous tissue flaps are raised on both sides. The third dorsal compartment is identified and opened along its entire length. The extensor pollicis longus (EPL) tendon is left in its sheath and not transposed. One must know the location of the EPL when incising the wrist capsule proximally. The wrist capsule is opened longitudinally and dissection performed to elevate the second and fourth compartments such that the second and fourth compartment tendons are maintained within the compartment. This exposes the scaphoid, lunate, triquetrum, capitate, and hamate.
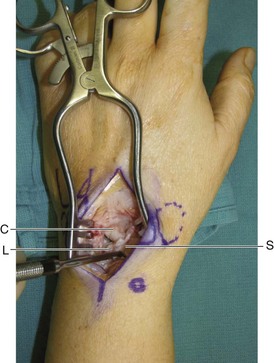
 Figure 88-3 shows a Freer elevator within the SL interval demonstrating a complete rupture of the SL ligament.
Figure 88-3 shows a Freer elevator within the SL interval demonstrating a complete rupture of the SL ligament.
Procedure
Step 1: Scaphoidectomy
 The scapholunate ligament is divided, and a sharp-edged Freer or an Obwegeser periosteal elevator is used to separate the scaphoid from the volar capsule. After adequate detachment of the volar capsule, a rongeur is used to hold the scaphoid and using a twisting motion, the surgeon removes the scaphoid as one piece.
The scapholunate ligament is divided, and a sharp-edged Freer or an Obwegeser periosteal elevator is used to separate the scaphoid from the volar capsule. After adequate detachment of the volar capsule, a rongeur is used to hold the scaphoid and using a twisting motion, the surgeon removes the scaphoid as one piece.
 The cancellous bone within the scaphoid is harvested for bone grafting.
The cancellous bone within the scaphoid is harvested for bone grafting.
Step 1 Pearls
A 0.062-inch K-wire inserted into the scaphoid to serve as a joystick can make dissection of the scaphoid from the volar capsule easier.
The entire scaphoid is removed in one piece and not in a piecemeal fashion. This ensures that portions of the scaphoid attached to the volar capsule are not left behind.